State of the Science: Implicit Bias 2018-2020
State of the Science: Implicit Bias 2018-2020Xiaodan Hu, PhD & Ange-Marie Hancock, PhD | Published 02:30 p.m. ET May 22, 2024.
Cite this article (APA-7): Hu, X., & Hancock, A. M. (2024). State of the science: Introduction to implicit bias review 2018-2020. The Kirwan Institute for the Study of Race and Ethnicity. https://kirwaninstitute.osu.edu/research/state-science-introduction-implicit-bias-review-2018-2020
The Kirwan Institute has a long history of aggregating and disseminating the latest research developments regarding implicit racial bias. We remain steadfast in our commitment to rigorously curating and making this work accessible as part of our land grant mission. In honor of Kirwan’s 20th anniversary and the 10th anniversary of the first Kirwan State of the Science, we are releasing three (3) State of the Science reports simultaneously (2018, 2019, and 2020) in a new virtual format. We will chronicle research developments in three general domains: education, healthcare, and law/criminal justice over this three-year period. Prior State of the Science reports are cited and linked where applicable throughout this page.
Introduction to State of the Science 2018-2020
Introduction to State of the Science 2018-2020The period from 2018 to 2020 was a memorable phase in our collective history, marked by profound cultural moments of change and awareness. These years witnessed racial and ethnic upheavals on an unprecedented scale, some of which were fueled and exacerbated by the COVID-19 pandemic, notably exemplified by instances of racism directed towards African American and Asian communities. In addition, long-standing systemic racial disparities were illuminated and intensified, culminating in widespread protests and demands for justice in 2020.
Perhaps the most searing reminder of these injustices was the death of George Floyd, a Black man, under the knee of a Minneapolis police officer. This disturbing incident, virtually witnessed by millions across the globe through social media and news outlets, sparked a profound sense of moral outrage. The event led to a flood of marches and demonstrations, transcending borders as communities around the world rallied together in solidarity around the anthem of “Black Lives Matter.” This international call for justice highlighted the universal resonance of George Floyd’s eulogy: “What happened to Mr. Floyd happens every day in this country, in education, in health services, and in every area of American life” (Sharpton, 2020).
This poignant statement, alongside the countless other incidents of racial injustice that took place during the 2018-2020 period, underscores the critical necessity of studying and addressing implicit bias against racial and ethnic minority groups. Using this lens empowers us to further understand how unconscious prejudices permeate our societies and contribute to negative outcomes for these populations. It is only through a deeper understanding that we can devise effective interventions that potentially reduce or effectively limit the impact of such biases.
Although the format of this State of the Science has changed, its aim has not: we reviewed and analyzed findings related to implicit racial biases research conducted in this three-year period to inform current dialogues and inspire further research that might help rectify the ongoing racial disparities illuminated throughout this review. While empirical research on implicit bias attends to a wide variety of demographic categories, this report follows Kirwan’s mission and standard practice of examining publications that pertain to implicit racial or ethnic bias. The purpose of this introduction is to provide a systematic review of the scholarly social science literature pertaining to the foundations of racial and ethnic implicit bias, which includes its definition, uses, and methodologies employed for empirical measurement of the phenomenon. Separate sections track research published in 2018, 2019, and 2020 across the domains of education, healthcare, and law/criminal justice.
Kirwan’s Approach to Defining Race and Ethnicity
The racial and ethnic classifications utilized in Kirwan’s 2018-2020 State of the Science reports adhere to the guidelines established by the 1997 Office of Management and Budget (OMB, 1997). It is also important to acknowledge that approaches to defining racial or ethnic categories have shifted and changed over time. For example, the US Census has allowed respondents to mark more than one racial category in the 2000, 2010 and 2020 census efforts, which was previously forbidden. Our approach to reviewing the scholarship published from 2018-2020 utilizes the OMB and Census approaches that were applicable during this timeframe. As aggregators of the research, we cannot control the racial and ethnic classifications employed by the original authors. This means not all racial and ethnic groups are studied or mentioned in recent publications, which itself is a research finding that emerges from this effort. That said, we are committed to ensuring consistency and coherence in the terminology used throughout our reports to enhance reader comprehension and facilitate a more accessible reading experience.
American Indian or Alaskan Native. An individual who has origins in any of the indigenous peoples of North America and South America (including Central America) and maintains their cultural identity through tribal associations or attachment with their community.
Asian. An individual with origins in any of the original populations of the Far East and Southeast Asia, or the Indian subcontinent including, for instance, Cambodia, China, India, Japan, Korea, Malaysia, Malaysia, Pakistan, the Philippine Islands, Thailand, and Vietnam.
Black. An individual with origins in any of the Black racial groups of Africa.
Hispanic or Latino. An individual with a cultural or ancestral background linked to Mexican, Puerto Rican, Cuban, Dominican, Central or South American, or other Spanish culture or origin, irrespective of their race.
Native Hawaiian or Other Pacific Islander. An individual having origins in any of the indigenous peoples of Hawaii, Guam, Samoa, or other Pacific Islands.
White. An individual with origins connected to the original peoples of Europe, North Africa, or the Middle East.
Key Definitions and Concepts
Implicit bias is defined as the set of attitudes or stereotypes that affect our cognition, affect and behavior in unconscious and automatic manner (Blair, 2002; Rudman, 2004). Implicit biases can be either positive or negative, and are activated involuntarily without an individual’s intention, awareness, or control. Implicit biases are pervasive; every individual is susceptible to them, including children and those with avowed commitments to impartiality (Nosek et al., 2007; Rutland et al., 2005; Greenwald et al., 1998; Kang et al., 2011).
Both nature and nurture contribute to how our implicit biases are formed. Renowned scholar Jerry Kang contends that, “even if nature provides the broad cognitive canvas, nurture paints the detailed pictures – regarding who is inside and outside, what attributes they have, and who counts as friend or foe” (Kang, 2012, p. 134). Indeed, our implicit biases are often developed as a result of mental associations formed by the direct and indirect messages we receive from our social environment, including those from parents, siblings, school environment, and the media. These messages are often about different groups of people, where certain identity groups are paired with certain characteristics (Nosek et al., 2007). For example a long line of research has documented media programming excessively portrays Blacks as criminals (e.g., Dixon & Linz, 2000; Gilens 2000; Gilliam 2000). After constantly being exposed to such messages, we may begin to associate a group unconsciously and automatically with certain characteristics, regardless of whether these associations actually reflect the truth of reality (Hancock 2004; Mendelberg 2001; Winter 2008). Implicit forms of bias also differ from more explicit forms, such as beliefs and preferences, which individuals are generally consciously aware of and can, if they choose to, identify and communicate to others (Daumeyer et al., 2019; Dovidio & Gaertner, 2010).
There are a few key types of mental associations that are frequently studied in conjunction with implicit bias. Infographic below illustrates both how they relate to each other and how they relate to implicit bias. Where it’s helpful we also provide some examples of each concept.
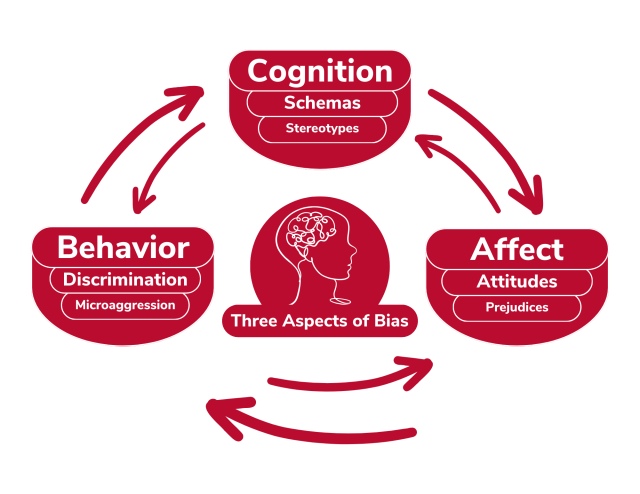
- Schemas can be described as mental frameworks that represent one’s understanding of an object, person, or situation, encompassing knowledge of its attributes and the connections between those attributes (Manstead et al., 1995). These mental structures are abstract, capturing common elements across various instances and serve to simply the complexities of reality. Schemas serve primarily as a guide for processing new information by setting up expectations about the type of information that will follow, linking specific details of a stimulus to a broader concept, and filling in any gaps in our understanding. There are five (5) primary types of schemas: person schemas (e.g., what a figure skater looks like), self-schemas (e.g., I am adventurous and outgoing), role schemas (e.g., nurses are caring), event schemas or scripts (e.g., going to a restaurant involves the sequence of reading the menu, ordering, eating and then paying the bill), and content-free schemas that contain information process rules instead of specific content (e.g., you never trust what your cousin says, regardless of what they actually say).
- Stereotypes are societally shared beliefs or abstract mental representations that we associate with social groups and their members (Blair, 2002; Greenwald & Krieger, 2006; Manstead et al., 1995) regardless of whether they are factually accurate. Stereotypes are sometimes described as “group schemas” or “group prototypes.” For example, Asians are commonly stereotyped as being proficient in math, while the elderly are often stereotyped as being feeble. Regardless of the valence (i.e., positive, neutral, or negative), these associations generally can be automatically accessed because they are routinized in our lives (Rudman, 2004). It is worth noting again here that stereotypes are not necessarily empirically valid and may reflect associations that we would consciously disapprove of (Reskin, 2005).
- Attitudes refer to psychological tendencies that involve the evaluation of a specific object or entity (Manstead et al., 1995). These evaluative feelings can range from having a positive, negative, or neutral stance towards a subject. Attitudes are often influenced by a person's beliefs, experiences, and values as well as factors like culture, social norms, and media representations. Importantly attitudes can change over time as people encounter new experiences or receive new information (Greenwald & Krieger, 2006; Kang, 2009).
- Prejudices are defined as antipathies “based upon a faulty and inflexible generalization” (Allport, 1954, p.9). Notably this key concept includes actions and not simply mental representations. Prejudice is characterized as holding derogatory attitudes or beliefs, expressing negative affect, or displaying hostile or discriminatory behavior toward an individual based on their group membership, which is associated with negative attributes assigned by the perceiver (Manstead et al., 1995). Prejudice has three components: a cognitive aspect involving beliefs about a particular group, an affective aspect involving feelings of dislike, and a conative aspect involving a behavioral inclination to exhibit negative actions or behaviors towards the targeted group (Dovidio et al., 2010).
- Microaggressions refer to subtle insults, either verbal, non-verbal, and/or visual, directed toward individuals or groups. Microaggressions are often automatic and unconscious (Solorzano et al., 2000). Put simply, they are brief, everyday exchanges that convey derogatory messages to people due to their membership in a minority group. These microaggressions are often delivered unconsciously through subtle snubs, dismissive looks, gestures, and tones during daily conversations and interactions. Despite their frequency, they are often dismissed or overlooked as being harmless. However, it is crucial to recognize that microaggressions have a detrimental impact on people of color. They diminish their performance in various settings by depleting their psychic and spiritual energy and creating inequalities (Sue et al., 2008).
We acknowledge the nuanced differences among these key concepts not least because the research we aggregated also acknowledged these differences. For example, Phills and colleagues (2020) examined the bidirectional causal relationship between implicit stereotypes and implicit prejudice. They found that valence changes in implicit stereotype (measured as semantic attributes associated with a group) influence in implicit prejudice. Moreover changes in implicit prejudice, defined as the valence (positive/negative) associated with the group, can also influence the extent to which it is associated with positive or negative semantic attributes. In other words, the two constructs are causally related concepts. In order to enhance simplicity and improve reader comprehension, the term “implicit bias” will be employed as a comprehensive label when evaluating articles that explore the impact of attitudes, stereotypes, prejudice, or schemas on our understanding, behaviors, and decision-making in an unconscious and automatic manner. We provide citations of the relevant research so that interested readers can go back to the original research for more detailed information.
How Did They Do That?
“To gain a better understanding of the appropriateness of using the term implicit bias as an overarching concept, a preliminary examination of the literature was conducted by two researchers, independently. While it was not a formal intercoder reliability check, this informal assessment aimed to evaluate the alignment between the articles selected for review and the definition of implicit bias provided earlier. Each researcher independently reviewed the same subset of 30 articles that did not explicitly employ the term “implicit bias,” from the overall pool of 291 articles. A consensus was reached through discussion to determine the criteria for identifying articles to be included in the review. Based on the established criteria, one of the researchers subsequently reviewed the remaining articles and made informed decisions regarding their inclusion in the review.”
Article Selection Strategy
Two rounds of literature searches were conducted for this report series covering articles in the English language published from January 2018 to December 2020. The search terms used were “unconscious,” “implicit,” “prejudice,” “bias,” and “stereotyp*” in combination with “rac*,” “ethni*,” and “color.” Three reviewers independently screened and selected eligible studies based on the title and abstract. Subsequently, the selected articles were re-evaluated by reading them in their entirety and categorized based on discipline. The inclusion criteria for the articles were as follows: 1) the articles should contain at least one finding or conceptual discussion related to implicit bias based on race or ethnicity; 2) peer-reviewed journal articles were given priority. Special cases such as articles from law journals, credible open-access journals and conference proceedings were also included. During manuscript preparation two members of the research team also performed an informal assessment that aimed to evaluate the alignment between the articles selected for review and the definition of implicit bias we discussed above. Subsequently, we verified whether the articles selected for discussion in these manuscripts a) substantively discussed implicit bias; b) fit within one of three categories – education, healthcare, or law/justice; and c) were academic articles published in either peer-reviewed or other academic journals. In sum, we analyzed a total of 133 articles; each subject report details the number of articles published between 2018 and 2020.
Empirical Measurement of Implicit Bias
The year 2020 marked the 25th anniversary of seminal publications that laid the foundation for measuring implicit biases. Over the past couple of decades, at least 20 different instruments (see Table 1) have been developed to measure implicit bias, beginning with Fazio and colleagues (1995), who validated the evaluative priming task (EPT). In the same year, Greenwald and Banaji’s (1995) reviewed implicit social cognition research, which served as the basis for the development of the Implicit Association Test (IAT; Greenwald et al., 1998). In the upcoming sections, we will provide a concise introduction to these two widely used measures of implicit bias. Although the EPT and the IAT have been the key instruments driving the upswing of research with implicit measures, they have distinct conceptual underpinnings (Payne & Gawronski, 2010). We will also briefly review other commonly employed measures that have been developed based on the foundation laid by the EPT and the IAT, including some physiological measures that have also been utilized to assess implicit bias.
Currently Available Implicit Measures as Summarized by Gawronski et al., 2020
| # | Measurement Instrument | Reference |
|---|---|---|
| 1 | Action Interference Paradigm | Banse et al. (2010) |
| 2 | Affect Misattribution Procedure | Payne et al. (2005) |
| 3 | Approach-Avoidance Task | Chen & Bargh (1999) |
| 4 | Brief Implicit Association Test | Sriram & Greenwald (2009) |
| 5 | Evaluative Movement Assessment | Brendl et al. (2005) |
| 6 | Evaluative Priming Task | Fazio et al. (1995) |
| 7 | Extrinsic Affective Simon Task | De Houwer (2003) |
| 8 | Go/No-go Association Task | Nosek & Banaji (2001) |
| 9 | Identification Extrinsic Affective Simon Task | De Houwer & De Bruycker (2007) |
| 10 | Implicit Association Procedure | Schnabel et al. (2006) |
| 11 | Implicit Association Test | Greenwald et al. (1998) |
| 12 | Implicit Relational Assessment Procedure | Barnes-Holmes et al. (2010) |
| 13 | Recoding Free Implicit Association Test | Rothermund et al. (2009) |
| 14 | Relational Responding Task | De Houwer et al. (2015) |
| 15 | Semantic Priming (Lexical Decision Task) | Wittenbrink et al. (1997) |
| 16 | Semantic Priming (Semantic Decision Task) | Banaji & Hardin (1996) |
| 17 | Single Attribute Implicit Association Test | Penke et al. (2006) |
| 18 | Single Block Implicit Association Test | Teige-Mocigemba et al. (2008) |
| 19 | Single Category Implicit Association Test | Karpinski & Steinman (2006) |
| 20 | Sorting Paired Features Task | Bar-Anan et al. (2009) |
| 21 | Truth Misattribution Procedure | Cummins & De Houwer (2019) |
Note. From Gawronski, B., De Houwer, J., & Sherman, J. W. (2020). Twenty-five years research using implicit measures. Social Cognition, 38(Supplement), 1-25. https://doi.org/10.1521/soco.2020.38.supp.s1
In general, many researchers have concluded that implicit and explicit measures capture distinct but related mental constructs (Nosek et al., 2007). The primary difference between implicit bias and other forms of bias revolves around the degree of consciousness. Explicit biases can be consciously registered and reported (Amodio & Mendoza, 2010). Implicit biases, however, arise outside of one’s conscious awareness and are not always congruent with an individual’s consciously held beliefs or attitudes (Graham & Lowery, 2004; Kang et al., 2012; Reskin, 2005). They may not necessarily reflect stances that one would explicitly endorse. While implicit and explicit bias are distinct concepts, they share similar impact: both mental constructs affect one’s actions, decisions and understanding.
In attempts to understand the differences between implicit and explicit bias, a number of other moderating factors have been identified to explain the divergent results captured by implicit and explicit measures (Rudman, 2004), including motivation to report explicit attitudes that correspond to one’s implicit attitudes (Dunton & Fazio, 1997; Fazio et al., 1995; Nier, 2005), the psychometric properties of the specific measurement techniques (Cunningham et al., 2001; Greenwald et al., 2003) and social desirability concerns (Dunton & Fazio, 1997; Nier, 2005; Nosek & Banaji, 2002).
Rudman’s (2004) work elucidates five factors that are more likely to influence the development of implicit biases than explicit ones. The first factor pertains to early experiences that may lay the foundation for our implicit attitudes, whereas explicit attitudes are influenced more by recent events. Furthermore, affective experiences tend to have more impact on implicit orientations than self-reports. She also listed cultural biases and balance principles as key factors that shape implicit biases. While the above-mentioned four factors were already established in the literature, Rudman adds a fifth factor for consideration, namely the self. According to Rudman (2004), it may be challenging to have implicit associations that are detached from the self, whereas controlled evaluations may enable more objective responses. If the self is a primary cause of implicit orientations, it is likely because individuals tend not to view themselves impartially, and this partisanship can then shape evaluations of other objects that are (or are not) related to the self.
The difficulties associated with measuring implicit bias arise in part due to its automatic and unconscious nature. Conventional self-report measures of bias rely on introspective and conscious reports regarding one's experiences and beliefs, which are indirect methods for assessing implicit bias. Additionally, impression management, or social desirability concerns, can undermine the validity of self-report measures. It is of particular concern when the target of measure is related to bias, as the desire to be perceived positively can lead people to alter their self-reported beliefs and attitudes to appear more impartial (Amodio & Devine, 2009; Dovidio et al., 1997; Fazio et al., 1995; Greenwald & Nosek, 2001; Greenwald et al., 2009; Nier, 2005; Nosek et al., 2007). This inclination towards impression management can compromise the validity of self-reports, especially when they are questioned on socially or politically sensitive issues such as intergroup or interracial behaviors (Dovidio et al., 2009; Greenwald & Nosek, 2001; Greenwald et al., 2009). Due to these limitations, self-reports are generally considered insufficient for capturing all dimensions of individual prejudice (Tinkler, 2012).
The Evaluative Priming Task (EPT)
The development of the EPT was guided by the notion that attitudes are represented in memory as associations of varying strength for object evaluation (Fazio, 2007). This view suggests that encountering an attitude object may automatically activate its associated evaluation via the spread of activation to the extent that the association between the two is sufficiently robust. For example, Fazio et al. (1995) conducted a study that explored the effects of priming participants with photographs of black and white undergraduates. During the study, participants were presented with an evaluative adjective, such as “pleasant” or “awful,” and their primary task was to indicate the connotation of the adjective as quickly as possible. A photo was briefly presented prior to each target adjective, with participants instructed to attend to the faces for later identification. The study was presented to participants as a cover story in which judgment of word meaning was portrayed as an automatic skill that should not be disturbed by the additional task. The results of this study indicated that Black and White faces had different effects on participants’ response time in indicating the connotation of the target adjective. Compared to white faces, black faces facilitated the response to negative adjectives and disrupted the response to positive adjectives. This pattern suggested that, on average, negativity was automatically activated by the black primes (Fazio& Olson, 2003). In this vein, the EPT was seen as an “unobtrusive” measure of attitudes, capturing unintended expressions of attitudes that are difficult to regulate, or that individuals may be unwilling to reveal on explicit self-report measures (Gawronski et al., 2020).
The Implicit Association Task (IAT)
Unlike the focus on unintentional expressions of attitudes that are challenging to regulate, the creation of the IAT was guided by studies on implicit memory. This approach proposed that memories of past experiences could impact responses even when they were inaccessible to introspection (Gawronski et al., 2020). In practice, the IAT gauges the degree of association between a target concept and an attribute dimension by measuring the time it takes for participants to utilize two response keys, each with a dual meaning. The participants’ task is to classify stimuli as they appear on the screen, such as categorizing names (e.g., “Latonya” or “Betsy”) as typical of blacks or whites. For example, race is the target concept, and the keys are labeled “black” and “white” in Greenwald et al.’s (1998) IAT on racial attitudes. Participants then categorize a range of words with clearly valenced meanings (e.g., “poison” or “gift”) as pleasant or unpleasant, which constitutes the attribute dimension.
During the critical phase of the study, the two categorization tasks are combined. Participants perform this combined task twice - once with one response key signifying Black/pleasant and the other labeled White/unpleasant, and once with one key indicating Black/unpleasant and the other White/pleasant - in a counterbalanced order. The main question is which response mapping participants find easier to use. In the Greenwald et al. (1998) study, participants were much quicker at responding when Black was paired with unpleasant than when Black was paired with pleasant. On average, participants found it easier to associate the target concept Black with the attribute unpleasant than with the attribute pleasant, which can be interpreted as indication of implicit racial bias.
Over the past decades, at least 20 different instruments (see Table 1) have been developed to measure implicit bias. Among these instruments, the IAT (#11) and the Single Category Implicit Association Test (SC-IAT; #19) are the most common measures used for the assessment of implicit biases and self-concepts. Most recently the IAT was found to have a higher accuracy of predicting behavioral choices over the SC-IAT, regardless of the scoring procedure (Epifania et al., 2020).
Additional implicit measures have been developed based on the groundwork laid by the EPT and the IAT. Two noteworthy examples include the Extrinsic Affective Simon Task and the Go/No-Go Association task. The former was developed as an affective variation of the spatial Simon task to measure attitudes implicitly (De Houwer & Eelen, 1998; De Houwer, 2003). During this task, participants must discriminate between the stimuli (e.g., noun/adjective or man-made/natural) by responding “positive” for one category and “negative” for the other. As the stimuli themselves have varying levels of associated valence, this process produces both evaluatively congruent trials, where the stimulus’s valence and its related category signal the same response (e.g., responding “positive” to “flower” as it is a noun), and evaluatively incongruent trials, where response competition arises (e.g., responding “negative” to “happy” as it is an adjective). The Go/No-Go Association Task was introduced by Nosek & Banaji (2001). It is a modified version of the IAT that eliminates the need for a contrast category. During the task, participants react to stimuli that symbolize the target and attribute categories as “good,” but take no action in response to other stimuli. The time taken to respond, or any errors made, are then compared to a block of trials where participants must respond to items that represent the target category and “bad.”
Several physiological methods have also been used as implicit measures of implicit bias. These diverse approaches share a common goal: to estimate the construct of interest without requiring a verbal self-report from the participant. The primary advantage of these indirect estimates is that they are less likely to be influenced by social desirability concerns. In many cases, participants may not even be aware that their attitudes, stereotypes, and so on are being measured until after a “debrief” session with the researchers, which is a common strategy used to make sure that accurate results are obtained while preserving the ethical standards of conducting human subjects research that informs participants of their rights and preserves said rights.
The seminal research in a related field experimented with a variety of physiological measures. Vanman et al. (2004) employed facial electromyography (EMG) to investigate racial prejudice. Both Phelps et al. (2000) and Hart et al. (2000) used functional magnetic resonance imaging (fMRI) to study amygdala activation as an indicator of racial evaluation. Eyeblink startle response to Black and White faces has also been used for this purpose (Phelps et al. 2000, Amodio et al. 2003). Cardiovascular reactivity measures, indicating challenge or threat, have been utilized to examine responses to interactions with Black individuals and others who face stigma (Blascovich et al. 2001). Furthermore, Cacioppo and colleagues have applied event-related brain potentials as a real-time measure of categorizing stimuli as positive or negative (e.g., Cacioppo et al. 1993, Crites et al. 1995, Ito & Cacioppo, 2000).
While these physical measures can effectively identify involuntary responses to stimuli, they also present challenges to implement, unlike the more broadly accessible online tests. The utilization of psychophysiological measures can demand significant time, infrastructure, and money. Therefore, these strategies may not be readily accessible to all researchers. When selecting an appropriate implicit bias measurement tool, we recommend a careful review of the strengths and drawbacks of each measure, including attention to the target concept of interest (e.g., stereotypes, schema, attitudes) to make informed decisions regarding the most suitable measure for their specific research/training objectives.
Facial Electromyography (EMG)
A technique used in the field of psychophysiology that measures the electrical activity produced by muscles in the face. This technique is valuable for examining implicit bias conveyed through emotional expressions. For example, EMG can be recorded from sites corresponding to muscles used in smiling, which is an indicator of positive emotions. In a study that looked at the preferences of White college students when choosing hypothetical candidates for a fellowship, participants exhibited higher levels of EMG activity in their cheek muscles when viewing pictures of White applicants compared to Black applicants. Elevated cheek EMG activity signals more positive emotions, suggesting that the participants may have an implicit bias in favor for White applicants (Vanman et al., 2004).
Functional Magnetic Resonance Imaging (fMRI)
A specialized technique that measures and maps the brain’s activity. When a brain region is more active, it consumes more oxygen, leading to a series of hemodynamic responses that fMRI can capture and visualize. Based on this mechanism, fMRI focuses on measuring changes in blood flow to particular areas of the brain as an indicator of increased neural activity. This allows researchers to understand how different cognitive tasks or stimuli engage specific brain regions. For example, activation in the amygdala, a small structure in the medial temporal lobe known for emotional learning and memory, has been linked to racial evaluation. Phelps and colleagues (2000) found that activation in the left amygdala is correlated with implicit bias shown through the IAT reaction time measure.
Pervasiveness of Implicit Racial Bias
Implicit racial bias has been found across different racial groups (Nosek et al., 2007) across a wide variety of countries. Nosek and colleagues were the first to conduct a large-sample study on the pervasiveness of implicit racial biases. Based on the data gathered from over 2.5 million IATs and self-reported surveys between 2000 and 2006, they found that about 68% of participants exhibited implicit racial bias against Black/dark-skin individuals, and 14% exhibited the reverse. It is worth noting that Black participants were the only group that, on average, did not show an implicit preference for White individuals. When examined by racial group, White participants displayed the strongest implicit pro-White preference. American Indians, Asians, Hispanics, members of multi-racial groups, and those who identified as “other” also displayed similar implicit racial preference at medium to large levels (Nosek et al., 2007). Nosek and colleagues also examined implicit associations of Blacks and Whites with weapons and harmless objects (e.g., umbrella, keys, or toothbrush). Approximately 72% of the sample showed strong associations of Black individuals with weapons and White individuals with harmless objects. While evidence of implicit bias associating Blacks with weapons was comparatively weaker among Black participants in comparison to other racial groups, the effect was still notable and relatively strong according to conventional effect size standards.
The target of negative implicit racial bias is not limited to Blacks. Two IAT instruments were designed to measure the implicit associations of ethnic-national groups. Specifically, they focus on determining whether Asian Americans or native Americans are more easily associated with the attribute of Foreign versus White Americans with American. Nosek and colleagues (2007) found that, on average, participants demonstrated a higher ease in associating White faces with the concept of “American,” and Asian or Native American faces with the notion of “Foreign,” rather than the reverse. This association, referred to as the Asian stereotype, was observed in 61% of the sample, while the Native American stereotype was observed in 57% of the sample.
When using the IAT instrument, Nosek and colleagues (2007) found that this measure detected stronger bias in people than the self-report measures. Specifically, they used a statistic called “Cohen’s d” to measure how far from a “neutral” standpoint people’s racial attitudes were in their nationally representative sample. While explicit self-report measures showed that people only had a small to medium level of preference for White (d = 0.31), the race attitude IAT for the same respondents revealed a much higher level of implicit preference for White (d = 0.86, more than twice the self-report score). If we were to translate these findings into a “normal” statistical distribution, we would predict that as many as 54.4% of individuals may explicitly admit to having a preference for White individuals. However, Nosek and colleagues’ empirical findings document a substantially larger proportion, 74.5%, who actually hold this preference for White individuals at an implicit level.
Mitigation Strategies for Implicit Bias
Although there was widespread belief prior to 2000 that implicit biases were difficult to change (Greenwald & Lai, 2020), there are findings showing that the unconscious attitudes or stereotypes we have formed can be “unlearned.” This means that implicit biases are malleable and can be replaced with new mental associations through interventional efforts (Blair et al., 2001; Blair, 2002; Dasgupta & Greenwald, 2001; Dasgupta, 2013; Roos et al., 2013). Such findings are important for providing support particularly to those individuals who might score on an EPT or IAT as having a biased preference but who do not think of themselves as biased or racist. We review general findings here; we also chronicle documented mitigation strategies pertaining to each subject category (education, healthcare, law/criminal justice) at the end of each State of the Science report.
Research on racial attitudes conducted by Fazio and colleagues has identified three distinct types of individuals, characterized by the automatic processes they engage in and their subsequent efforts to counter or control those evaluations (Fazio et al., 1995). The first group consists of individuals who are non-prejudiced; these individuals do not exhibit the activation of negative attitudes towards a particular racial group. The second group encompasses individuals who are genuinely prejudiced, as they experience negative automatic associations but make no attempts to counter or control the expression of those associations. The third group comprises individuals who may experience negative automatic associations, but they are motivated to actively counter such sentiments. Individuals in this last group, who seek to mitigate the role of implicit racial biases in their overt actions or behaviors can pursue intentional actions at either the personal (internal) or the situational (external) level. Each type of influence has been documented to shape the conditions under which implicit racial biases are likely to affect behavior.
Personal Factor 1: The Role of Motivation
Motivated individuals have the capacity to exert influence over the automatic operation of stereotypes and biases (Blair, 2002). Dunton and Fazio (1997) investigated the influence of motivation on controlling biased reactions and identified two sources of motivation: a concern with appearing prejudiced and a desire to avoid conflicts or disagreements about one’s thoughts or positions. Their findings suggested that individuals with low motivation to control biased reactions were more likely to provide accurate self-reports of racial attitudes. Devine et al. (2002) further explored the impact of motivation on implicit and explicit biases, concluding that explicit biases were moderated by internal motivation, while implicit biases were influenced by the interaction of both internal and external motivation.
Devine et al.’s finding is consonant with that of Irene Blair. Blair (2002) identified two individual (internal) level interventions and one situational (external) intervention that can potentially mitigate implicit bias. The internal factors involve examining the manipulations of the perceiver’s motivations, goals, and strategies during the process in which implicit bias arises. On the other hand, the external factor identified by Blair focuses on changes in the context surrounding the stimulus or variations in the attributes of group members.
Individuals who possess high motivation have the ability to influence the automatic activation of stereotypes and bias (Blair, 2002). When an individual’s self-image is threatened, they may automatically activate negative stereotypes in order to enhance their own appearance or discredit someone they dislike (Sinclair & Kunda, 1999; Spencer et al., 1998). Conversely, they can also automatically suppress negative stereotypes and activate positive ones when it benefits their self-image (Sinclair & Kunda, 1999). Automatic stereotypes and bias can be influenced by the social demands of a situation and the nature of one’s relationship with others. For example, White individuals may moderate their automatic bias when interacting with a Black person, particularly if they are in a subordinate position (Lowery et al., 2001; Richeson & Ambady, 2001). They may also adjust their automatic stereotypes if those stereotypes conflict with social norms (Sechrist et al., 2001).
The concept of overcorrection, where individuals compensate for their biases by displaying exaggeratedly positive or negative responses that conceal their true attitudes, has also been investigated. Dunton and Fazio (1997) suggested that highly motivated individuals who aim to control prejudiced reactions might overcompensate for their automatically activated negativity, resulting in more positive judgments than those with activated positivity.
Personal Factor 2: Promotion of Counter Stereotypes
It is argued that individuals who perceive stereotypes have the ability to actively foster counter-stereotypic associations. By doing so, they can potentially undermine the influence of implicit stereotypes in the process of information processing. Promotion of counter stereotypes can be achieved through tasks such as priming of counterstereotype expectancy, mental imagery, and exposure to counterstereotypic group members (Blair & Banaji, 1996; Blair et al., 2001; Dasgupta & Greenwald, 2001). To examine the effect of counterstereotype expectancy on implicit bias, Irene Blair and Mahzarin Banaji (1996) conducted a sequential priming task, which assesses automatic associations by measuring how a briefly presented stimulus (prime) influences the response time to a subsequent stimulus (target). Half of the participants were instructed to anticipate prime-target trials that aligned with stereotypes, while the other half were informed to expect counterstereotypic trials. However, in reality, all participants experienced both stereotypic and counterstereotypic trials, with the anticipated trial type appearing only 63% of the time. The results of this study revealed that the counterstereotype expectancy significantly lowered levels of automatic stereotypes than the stereotype expectancy.
The effect of mental imagery was examined through tests targeting implicit gender stereotypes. Blair and colleagues (2001) instructed the participants to spend around 5 minutes to create a mental image of a strong woman, which is counterstereotypic to the traditional stereotype, and then complete an automatic gender stereotype test. Participants who engaged in the counterstereotypic mental imagery exhibited substantially weaker automatic stereotypes compared to participants in the control groups, which included those who attempted to suppress their stereotypes on their own.
The exposure-to-counterstereotypic-group-members mitigation strategy takes a somewhat different approach. A group of participants were exposed to either a) admired African Americans and disliked White Americans, b) disliked African Americans and admired White Americans, or c) nonracial control stimuli. Following the exposure, the participants took IAT automatic racial bias measures both immediately and 24 hours later (Dasgupta & Greenwald, 2001). The study found that exposure to positive Black group members reduced automatic bias against Blacks compared to exposure to negative group members or to control stimuli. It is also worth noting that this effect continued to be significant after 24 hours. While Dasgupta and Greenwald (2001) believe that this effect is likely to diminish after an extended hiatus, these findings remain significant as they challenge the assumption that automatic racial attitudes, ingrained through long-term socialization, are unchangeable.
One potential concern the researchers emphasized about their results regards the possibility that when individuals are exposed to strongly positive and negative exemplars of a particular stereotype, they might categorize these exemplars as “exceptions to the rule” and adjust their attitudinal response accordingly before expressing it. This observation aligns with studies on stereotypic belief revisions, which demonstrate that when confronted with evidence, explicitly held stereotypes can remain firm if the new evidence or exemplars are perceived as atypical (Bodenhausen et al., 1995; Kunda & Oleson, 1995; Rothbart & John, 1985; Weber & Crocker, 1983). As such, instead of revising the original stereotype, new cognitive categories are created to accommodate these counterstereotypic exemplars, a phenomenon known as subtyping. However, Dasgupta and Greenwald (2001) contend that this effect is less likely to manifest when individuals do not have ample cognitive resources to reflect on and recategorize these counterstereotypic exemplars. This perspective is supported by the findings of Dasgupta and Greenwald’s study, where exposure to counterstereotypes reduced implicit, but not explicit, stereotypes against Black individuals. The researchers therefore cautioned that care must be taken to ensure that this type of exposure doesn’t label the counterstereotypic exemplars as mere exceptions, which would inadvertently perpetuate the original stereotype.
Personal Factor 3: Group Membership and Identity
Perceptions of group membership and identity are another personal factor that can influence one’s implicit bias. Categories such as race, gender, and age can be perceived almost instantaneously (Cikara & Van Bavel, 2014; Ito & Bartholow, 2009). Ingroups, whether they exist in real life or are artificially created for an experiment, can result in attitudes and behaviors of favoritism (Pinter & Greenwald, 2011; vanKnippenberg & Amodio, 2014). Simon and Gutsell (2020) interrogated this phenomenon utilizing the minimal group paradigm developed by Tajfel, Billig, Bundy and Flament (1971). This paradigm allows researchers to create experimental social categories that participants have never encountered before, enabling control over individual experiences, motives, and opinions. Participants in this study were evenly assigned to two minimal groups with arbitrarily created racial names. Researchers found that knowledge of arbitrary group membership led participants to humanize and show implicit bias favoring their ingroup members of the minimal group, despite the cross-cutting presence of race. This finding demonstrates that even within minimal groups, the consequences of implicit racial bias can be overcome through recategorization.
To further comprehend the underlying dynamics of this effect, Fritzlen and colleagues (2020) conducted two studies exploring the boundary conditions of the reclassification effort. They first examined whether learning of an identity-implying similarity with an outgroup could influence once’s implicit bias towards that outgroup. One of the identity-implying similarities they used in the study was genetic overlap with an outgroup. Their first study found that White participants who were made to believe that they had greater than average genetic overlap with African Americans showed decreases in implicit bias against that racial group. In a follow-up study, the researchers explored whether this effect holds in the context of sexual orientation identity. In this study, heterosexual participants were led to believe that they exhibited same-sex attraction and their implicit bias against homosexual individuals were measured. The findings showed that heterosexual participants’ implicit biases against homosexual individuals were reduced only if respondents believed that sexual orientation was biologically determined. Thus, Fritzlen and colleagues (2020) concluded that learning of an identity-implying similarity with an outgroup can reduce implicit bias if that group membership is perceived as immutable.
These findings hint at a broader implication that aligns with the intergroup contact theory, which suggests that direct contact between members of different social or cultural groups can be effective in reducing prejudice and conflicts between groups (e.g., Allport & Kramer, 1946; Lee & Humphrey, 1968; Pettigrew & Tropp, 2006). For instance, Kephart (1957) found that White police officers in who had worked with Black colleagues differed substantially from other White policemen on the force. They had fewer objections to teaming with a Black partner and taking orders from qualified Black officers. Combined with the evidence for minimal group reclassification effect on implicit bias (Frizlen et al., 2020), this suggests that enhancing awareness of shared group membership or identities, even arbitrary ones, could serve as a strategic approach to fostering positive intergroup relations and reducing implicit biases.
Furthermore, having positive intergroup contact has been shown to have potential positive influence over implicit bias as well in both virtual and real-life settings. Early behavioral studies found that people are better at recognizing faces from their own race compared to faces from other racial targets (Meissner & Brigham, 2001), a phenomenon dubbed as “the own race bias.” Following this line of research, Farmer and colleagues (2020) investigated whether positive intergroup contact can moderate the implicit bias in face perception using fMRI. In their study, White participants with a varied range of contact experiences with Blacks were first selected through a pre-task questionnaire. During the fMRI scan the selected participants completed an individuation task (favorite vegetables) and a social categorization task (above or under 25 years old) while viewing the faces of both Black and White strangers. The fMRI results showed that more frequent positive contact with Black individuals increased activation for Black faces in the social categorization task. This finding shows that quality of intergroup contact is also a key factor in processing out-group faces and reducing the own-race face bias. Improving the quality of intergroup contact is something individuals who are motivated to mitigate their biases have control over in their personal lives.
Contextual Factor 1: Configuration of the Cues
One important area for mitigation efforts focuses on how individuals interpret cues provided to them. Two types of studies have ensued: impression formation and perspective taking. In the classic impression formation studies conducted by Asch (1946), participants were given the task of forming impressions of an individual based on a set of traits such as skillfulness, industriousness, and intelligence. The presence of the trait “warm” or “cold” on the list had a significant impact on the impressions formed by the participants, leading to notable differences in their evaluations. Researchers argued that such fluidity in meaning may also be observed in automatic processes such as implicit stereotypes and biases (Blair, 2002). For instance, Macrae et al. (1995) conducted a study that highlighted how even a slight contextual change can exert a notable influence on automatic stereotypes. In their experiments, all participants were exposed to a Chinese woman, and subsequent measurements of automatic stereotypes toward both Chinese individuals and women were taken using a lexical decision task. In one condition, the Chinese woman was observed applying makeup, while in another condition, she was seen using chopsticks. As hypothesized, Macrae et al. discovered that participants who witnessed the woman applying makeup exhibited faster responses to traits stereotypically associated with women and slower responses to traits stereotypically associated with Chinese individuals. Conversely, participants who observed her using chopsticks displayed the opposite pattern of responses. Despite the stimulus remaining the same, a minor alteration in the context resulted in a substantial change in the automatic stereotypes evoked by her presence. Similarly, the automatic attitudes triggered by the presence of the same Black individual can vary depending on the setting (Wittenbrink et al., 2001). For example, when a person is encountered on a city street, different automatic attitudes may emerge compared to when they are encountered inside a church. In general, city streets are often associated with more negative perceptions compared to the interior of a church, and similarly, Black faces tend to be perceived more negatively than White faces. It is important to note, however, that these qualities do not independently impact the automatic process. Instead, their effects are multiplicative, meaning that when a Black face is encountered in a city street context, the automatic negativity becomes particularly strong.
An individual’s capacity to take perspectives and to show empathic concerns are also significant predictors of their implicit bias (Patané et al., 2020). Researchers have theorized that bilingualism may enhance perspective-taking at early developmental stages, thus reducing the expression of social bias. Being raised with more than one native language is often considered an advantage as it diversifies the range of linguistic, social, and cultural experiences available to an individual (Singh et al., 2020). Singh and colleagues compared monolingual and bilingual children to examine whether bilingual individuals are as susceptible to racial bias as their monolingual counterparts. Results showed that bilingual individuals displayed less implicit bias against Blacks. Additionally, it is possible that bilingualism predisposes individuals to more frequent social encounters with outgroups (something we discussed in association with personal factor #2), which may also reduce implicit bias against members of an outgroup.
Kang and Falk (2020) explored perspective-taking via an fMRI study to investigate the relationship between individuals’ tendencies to engage brain regions that support perspective-taking and their implicit biases towards a stigmatized group. Their findings revealed that an intervention task that exercised one’s ability to make inferences about others’ mental states was able to reduce implicit bias. Therefore, the researchers argued that intervention strategies designed to enhance social cognitive processing could be effective in reducing people’s implicit biases against stigmatized individuals. Patané and colleagues explored a related perspective-taking question using immersive virtual reality (VR) technology to explore whether interventions tailored to increase perpective-taking can help to reduce implicit racial bias and the use of VR technology to design interventions to reduce implicit racial bias. The researchers had a group of White study participants embody a Black virtual body. They compared those who engaged in a cooperative activity with another Black avatar to those who engaged in a neutral activity. The results revealed that those who engaged in a cooperative activity with a Black avatar had lower IAT scores after the social interaction than those who engaged in a neutral activity with a Black avatar.
Collectively, these findings indicate that automatic perception relies on the configuration of various stimulus cues, and even small changes can lead to remarkably different outcomes. It highlights the sensitivity of automatic processes to contextual factors and the potential for subtle modifications to have a profound impact on perception (Blair, 2002).
Contextual Factor #2: Time
Time is a recognized factor that plays a role in decision-making and the ability of individuals to regulate their reactions. Studies have indicated that time pressures can create conditions in which implicit attitudes become evident, even when individuals make explicit efforts to control them (Kruglanski & Freund, 1983; Payne, 2006; Sanbonmatsu & Fazio, 1990). This suggests that under time constraints, implicit attitudes may manifest themselves despite individuals’ explicit attempts to exert control over them (Bertrand et al., 2005). This phenomenon could have important implications for professionals such as police officers and other authorities who must make split-second decisions in their line of work. For some of these professionals who already harbor implicit biases, making quick judgment may not necessarily alter their biases but rather make these biases evident through behavioral manifestations. Highlighting this, Payne (2005) conducted a study to examine participants’ implicit associations related to weapons and race. The findings revealed that individuals with more negative implicit attitudes towards Blacks exhibited a stronger bias associating weapon with them. In a subsequent analysis, Payne (2006) emphasized that a crucial component of intentional response control gets overshadowed when the focus is solely on automatic bias.
Rapid judgments do not alter individuals’ biases but instead allow these biases to manifest as overt behavioral errors when time is limited. For example, Gallo et al. (2013) found that the time pressure on a White referee before making a decision to punish a football player affected their level of discrimination against players who are foreign and non-White, signaling an increase in implicit racial bias. Time pressure also shapes medical decisions, potentially to the detriment of racial minority patients. Stepanikova (2012) found that when family physicians and general internists are under high time pressure, their implicit bias against Black and Hispanic patients results in less serious diagnoses for both groups and a reduced likelihood of specialist referrals for Black patients.
Contextual Factor #3: Cognitive “Busyness”
According to Reskin (2005), any factors that tax our attention, such as multiple demands, complex tasks, or time pressures, increase the likelihood of us resorting to stereotyping. Gilbert and Hixon (1991) investigated the influence of cognitive busyness on the activation and application of stereotypes. Their findings showed that cognitive busyness reduces the likelihood of stereotype activation. However, if a stereotype is activated, cognitive busyness increases the probability of applying that stereotype to the individual(s) in question. Payne (2006) conducted an experimental study to examine the relationship between bias and cognitive overload, a state in which an individual’s working memory is overwhelmed by more information or tasks than it can effectively handle at a given moment. Payne found that cognitive overload leads to increased bias, which he attributed to individuals’ diminished control over their responses due to lack of cognitive resources. Furthermore, Bertrand et al. (2005) identified three conditions conducive to the emergence of implicit bias, including lack of attention to a task, time constraints or cognitive overload and ambiguity. In the health care setting, cognitive load may stem from stressful mental tasks, such as decision-making for multiple patients, as well as environmental factors such as overcrowding. Supporting the perspective put forward by Bertrand et al., Johnson and colleagues (2016) found that overcrowding and patient load indeed contributed to increases in physicians’ implicit racial bias. Additionally, despite unfounded concerns about non-White individuals being more likely to abuse opioids, Burgess et al. (2014) reported that male physicians were less than half as likely to prescribe opioids for pain management to Black patients compared to White patients when under high cognitive load. Similar evidence was found in the field of sports as well. The ambiguity of situations regarding infringements in football was found to affect the referee’s level of discrimination, which strongly points to the influence of cognitive busyness on the presence of implicit bias (Gallo et al., 2013).
Conclusion
This introduction to the research on implicit bias has summarized more than 25 years of empirical research to define racial/ethnic implicit bias, outline contributing factors, and offer evidence-based mitigation strategies for individuals motivated to change. It dedicated a crucial amount of attention to this latter subject given this burgeoning area of research. Please explore the 2018-2020 State of the Science reports by subject domain below to review the research trajectories in your preferred topic of interest by clicking on the links below. Each domain features a segment dedicated to the advances in scholarship from 2018, 2019, and 2020, respectively.
Acknowledgements
The Kirwan Institute would like to extend our heartfelt gratitude to various individuals who have contributed to the development and completion of this project. Earlier parts of this project began under the leadership of interim director Dr. Beverly J. Vandiver, who supervised literatures searches by Preston Osborn, MSW; Laura Goduni, MPH: and Xiaodan Hu, PhD during the challenging times of a global pandemic. Their work served as a trusted guide for this work.
Former Kirwan program coordinator Adriene Moetanalo provided literature classification checks and editing, which have greatly enhanced the quality of this report, as have the creative talents of Kirwan student worker Chi Mutiso, who designed the infographics that so effectively communicate the key terms, findings, and insights of this research.
Each of these individuals’ hard work enabled us to present a more informed analysis. They all played pivotal roles at critical points in the realization of this project, and for that we are incredibly thankful.
Implicit Bias in Education: 2018
Implicit Bias in Education: 2018In 2018, implicit racial bias research in education continued its expanded attention to the impact of implicit biases on students and education policy. Our review includes nine (9) studies published in 2018. Ranging from how educators’ unconscious stereotypes may lead to the dehumanization and marginalization of youth of color, to disparities in disciplinary actions and evaluations of learning skills, these studies provide an in-depth look at the pervasiveness of implicit bias in educational settings.
In educational settings, implicit bias has been well-documented in the literature as a contributing factor to differences in teacher-student interactions (Okonofua & Eberhardt, 2015; Warikoo et al., 2016). Beyond the classroom, however, implicit racial biases potentially held by school administrators, such as principals and vice principals who are also an integral part of education systems, are rarely examined. The impacts of implicit racial biases manifest students’ mental/behavioral/health and academic outcomes, as well as aggregated racial disparities in school discipline and underrepresentation of racial and ethnic minoritized populations across various academic fields. Understanding these biases, their manifestations, and impacts, can expand our ability to creatively address the persistent challenges implicit biases present in educational contexts.
Impact on Students
According to new research published in 2018, the detrimental effects of implicit racial biases on students can be classified into two subcategories: societal and institutional devaluation and negative academic outcomes. We take each in turn.
Prior research documents the ways in which implicit bias may lead to a dehumanization process where youth of color are perceived as older, less innocent, and therefore more accountable for their actions than their White peers of the same age (Goff et al., 2014). This dehumanization process could result in reduced or absent social protection in school settings, making children of color more susceptible to punitive measures and less likely to be given chances to rectify their wrongdoings (Goff et al., 2008). Building on the earlier work of Philip Goff (2008; 2014); Matteo Forgiarini and colleagues (2011); Joshua Correll and colleagues (2002); and Walter Gilliam and colleagues (2016), Annamma and Morrison (2018) argued that young individuals of color are subjected to the negative impacts of implicit bias through dehumanization, pain minimization, and fear maximization. Citing empirical evidence, Annamma and Morrison detailed in their discussion the process by which youth of color as young as 12-years old are dehumanized while their pain may be overlooked. The outcomes can be fatal for some, as seen in the case of Tamir Rice, who was shot by Cleveland police while playing with a toy gun. Meanwhile, others may endure less direct but still damaging forms of violence by adults in authority.
The role of fear maximization and dehumanization also affects subgroups of the United States population in particular ways. Anthony Brown (2018) offered a thorough review of theological, scientific, and social science discourses where the construction of race has been shaped in relation to Black males. The impact of these biased practices, according to Brown, originates from the durable racial discourses of power that persistently portray Black males as feared and dangerous. In this way Brown also emphasizes the connections between fear maximization, dehumanization, and implicit racial bias against Black males in schools and society.
A second area of 2018 research focuses on the impact of implicit racial biases upon teachers’ evaluations of students’ learning skills. Building on the prior work of Lennard Davis’s critical disability theory (2013), Parekh and colleagues (2018) argued that it is important to examine the role of implicit racial bias in teachers’ evaluations of students’ learning skills and how it affects different communities. They suggested that critical disability theory is particularly relevant because it dissects how our society’s excessive emphasis on ability can unfairly label people, especially those from communities that often struggle with poverty and precarity. Their exploratory study of teachers’ perception of students’ learning skills across demographic and institutional factors drew data from Canada’s largest public board of education, which served approximately 246,000 students at the time of the study. The researchers examined the associations between students’ self-reported racial identity and the degree to which they were noted as having “Excellent” learning skills across achievement categories. The findings indicated that White students were typically the most likely to be given this high rating for their learning skills. On the other hand, despite being compared at similar academic levels, students self-identifying as Black were less likely to be recognized as having “Excellent” learning skills. The results imply that Black students, irrespective of their academic performance, are not perceived to embody core attributes implicitly valued by the educational system.
This 2018 study aligns with similar results found at the post-secondary level in earlier research. In a simulated setting that replicated teaching interactions involving college student participants who exhibited lower performance on a test, researchers discovered that White instructors showed stronger implicit associations favoring White individuals and harbored negative associations towards similarly situated Black individuals (Jacoby-Senghor et al., 2015). Another study examined implicit racial associations held by teachers concerning White and Arab individuals in the United States (Kumar et al., 2015). It was observed that teachers with implicit biases favoring White individuals and holding negative associations towards Arab individuals were less inclined to establish a culturally responsive classroom environment and facilitate the resolution of interethnic conflicts within the classroom.
Historically both the intention and assumption of the roles that teachers play in classrooms have been focused on teachers’ ability to promote egalitarian attitudes and foster harmony among individuals of different races. Teachers – particularly but not exclusively White teachers – have been found to play a significant role in perpetuating racial inequality that requires attention, intention, and mitigation (Ladson-Billings, 1994; Gershenson et al. 2016). Please see the Mitigation Strategies section of this report for research findings regarding successful interventions.
Systemic Impact
Having explored the intricate ways in which implicit bias can directly impact student outcomes, we now investigate how these biases further manifest in specific areas of the educational system. In the education sector, the role of implicit bias has been linked to racial disparities in school disciplinary actions. Racial disparities play a significant role in both K-12 educational outcomes like high school graduation rates and youth getting caught up in what is now commonly called the “school-to-prison pipeline.” The stakes, therefore, could not be higher for young people.
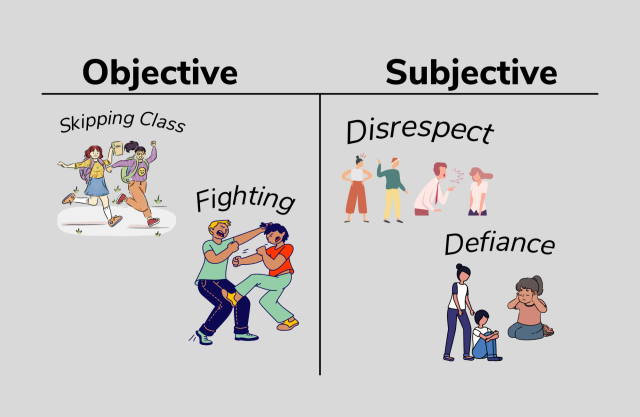
The first area of systemic implicit racial biases’ impact is school discipline. A vast amount of prior research suggests that disciplinary methods in schools affect students of color more than their peers (such as Wallace et al., 2008; Skiba et al., 2011; Hannon et al., 2013). A plethora of studies have found that certain student subgroups face a disproportionate amount of exclusionary discipline (Aud et al., 2011; Nowicki, 2018; U.S. Department of Education, Office for Civil Rights, 2015). Implicit racial bias is one of the contributing factors to this problem (Girvan et al., 2017; Goff et al., 2014), particularly under certain conditions, such as when teachers or administrators are making decisions that are ambiguous, demand fast judgement, or when they are physically or mentally drained (Kouchaki & Smith, 2014). Black students were found to be significantly more likely than White students to be labeled as troublemakers, their misbehaviors were more likely to be perceived as indicative of a pattern. Educators also showed a higher tendency to envision themselves suspending a Black student in the future compared to a White student. (Okonofua & Eberhardt, 2015). The role of implicit bias in school discipline becomes more evident when we examine the disparities for more subjective behavior infractions such as disruption, as opposed to objective infractions like theft (Skiba et al., 2011). Objective infractions are behaviorally defined and based on objective event (e.g., fighting, skipping classes) that often leaves a permanent product, whereas subjective infractions are defined vaguely and more open to subjective interpretation (e.g., defiance, disrespect; Skiba et al., 2002; Theriot & Dupper, 2010). A study of student discipline records from more than 1,800 schools unveiled that these disparities were largely due to racial differences in office discipline referrals for subjectively defined behaviors such as defiance (Girvan et al., 2017). In sum, the past 12 years of studies reveal a troubling trend of systemic unfair treatment of students of color attributable to implicit racial bias.
A second area of systemic implicit racial biases’ impact is the persistent underrepresentation of racially minority students in particular fields, including but not limited to STEM education (McGee, 2021). Two 2018 studies – one in chemical engineering and one in the humanities – explored this impact, as did a cross-disciplinary study of recommendation letters. Farrell and Minerick (2018) examined the stealth nature of implicit bias in the realm of chemical engineering education. They argued that the pervasive presence of implicit bias and stereotype threat creates an environment where educators tend to allocate their time and resources to those students they perceive as more likely to succeed. Such an environment is likely to generate self-fulfilling prophecies and to negatively impact students’ interest in a subject as well as their levels of effort. In the same vein, Holroyd and Saul (2018) provided a detailed discussion of implicit bias in the field of philosophy. The authors suggested that implicit biases might be part of the explanation for the persisting underrepresentation and marginalization of multiple groups in philosophy. For instance, Black PhD students and professional philosophers combined are merely 1.32% of philosophers in the U.S. (Botts et al., 2014). The authors further emphasized the gravity of the situation, noting how implicit biases perpetuate unjust societal structures.
The role of implicit bias is not only limited to direct interactions between educators and students, but it also permeates more indirect aspects of the education system such as recommendation letters. Letters of recommendation, often utilized to evaluate undergraduate students’ potential for success as research assistants, interns, or graduate students, can sometimes include implicit bias, thereby potentially impacting decisions and constraining opportunities for underrepresented minorities and students from non-research institutions. Houser and Lemmons (2018) employed a text analysis software to analyze 457 recommendation letters for undergraduates applying for an international research experience, aiming to identify any significant difference in the language used to depict students who were accepted versus those who were rejected. The findings indicate that recommendation letters for successful applicants depict the students’ productivity with more certainty and incorporate more student work quotes. Conversely, the letters for unsuccessful applicants contain more positive emotion and mention the students’ insight, but also include more discrepancy-associated words (e.g., should) and tentative statements (e.g., perhaps, maybe). The statistically significant results showed the White students tended to be described in relation to their cognitive ability, insightfulness, productivity, and perceptiveness while non-White students tended to be depicted in affective languages and positive emotions.
Taken together, research conducted in 2018 regarding the impact of implicit bias continues to document the deleterious effects of implicit racial bias on students of color as well as an aggregate impact that produces systemic racial disparities. Highlights from 2018 include a theoretical focus on the mechanisms of dehumanization and fear maximization directed at individuals of color. This was complemented by studies that explored the role of implicit bias in teachers’ evaluation, nuances in recommendation letters, and underrepresentation of racial and ethnic minority populations across various academic fields. These studies and critical analyses provide a more updated understanding of the scope of implicit racial bias in education, underscoring the urgency for the sector to take meaningful actions.
Implicit Bias in Education: 2019
Implicit Bias in Education: 2019While there has been an increase in racial and ethnic diversity within the United States, many still live in segregated communities (Logan, 2013). The connection between housing and education segregation further perpetuates inequality from early life through adulthood (Wells et al., 2016). The lack of resources in schools from impoverished and segregated districts exacerbates this vicious cycle of inequality (Rothstein, 2013; Wells et al., 2016). A study by McCardle and Bliss (2019) explored the connection between school segregation and implicit bias, revealing a significant correlation between one’s personal diversity experiences and their levels of implicit bias. Specifically, individuals with more diverse experiences demonstrated lower levels of implicit bias. The complex interplay between implicit bias and education settings served as a focus of burgeoning research, drawing academic attention from 2019 to the manifestation of implicit bias in multiple educational environments, including early childhood, higher education, and special education. In the following section, we will examine publications from 2019 that explore implicit bias in each of these environments.
Early Childhood Education
Shifting our focus to the foundational years, Perszyk and colleagues (2019) aimed to investigate the interplay between racial and gender biases in young children. Considerable evidence indicated that adults tend to evaluate Black men more negatively compared to Black women, White men, and White women (Kang & Bodenhausen, 2015; Navarrete et al., 2010; Purdie‐Vaughns & Eibach, 2008; Sidanius & Veniegas, 2000). This intersectional pattern was also evident in adults’ assessments of Black boys (Todd et al., 2016). Specifically, prior research observed that preschool teachers tend to direct their visual attention in a way that suggests they anticipate disruptions from Black boys more than from other racial and gender groups of children (Gilliam et al., 2016). Building upon this foundation, Perszyk et al. focused on preschool-aged children to investigate whether this intersectional bias pattern exists within young children. Utilizing both implicit and explicit measures, the researchers evaluated how 4-year-old children responded to images of children varying in both race (Black and White) and gender (male and female). The results revealed a consistent pro-White bias among children. Furthermore, implicit bias in children was also assessed in racially more homogeneous countries. Qian et al. (2019a) conducted their research to assess the developmental course of implicit bias in Chinese participants. Their study showed that children as young as four years old displayed implicit racial bias towards outgroup members. Setoh et al. (2019) conducted research into the correlation between racial categorization and implicit racial bias in Chinese and Indian preschool children. The study revealed that children’s capacity to classify faces by race was connected to their implicit racial bias, rather than their explicit racial bias. This implied that children’s subconscious racial bias is linked to their perceptual abilities, rather than their conscious convictions about race. Additionally, the study explicitly considered the assertion that actively teaching children about racial categories might actually increase the prominence of these categories and have unintended consequences.
Special Education
One article in our sample expanded the scope of implicit biases into special education. Building on prior research by Redfield and Kraft (2012), Oelrich (2012), and Fabelo et al. (2011), Dustin Rynders (2019) conducted an in-depth critical exploration of racial disparities in identification, discipline, service, and placement associated with special education. The author’s analyses highlighted evidence that Black students are disproportionately overrepresented in the more subjective disabilities categories such as having emotional disturbance and have a higher chance of being placed in restrictive settings (e.g., a separate, self-contained class; Redfield & Kraft, 2012). Furthermore, it was also found that White teachers refer a disproportionately high number of minority students to special education (Oelrich, 2012). These decisions could adversely affect minority students, given a previous report indicating that nearly 75 percent of special education students have faced suspension or expulsion at least once (Fabelo et al., 2011). Rynders identified implicit bias as one of the contributing reasons for these disparities.
Higher Education
Within the realm of higher education Robinson et al. (2019) compiled narratives delving into the experiences of women of color within a predominantly White academic institution. Through a synthesis of statements from both students and faculty, the article highlighted concerns related to the recruitment, retention, and support of minority faculty and students in higher education. The analysis also exposed the hurdles faced by women of color, such as microaggressions, tokenism, and underrepresentation in leadership roles. Robinson and colleagues argued that implicit bias is one of the key factors contributing to these challenges encountered by women of color. Furthermore, the authors also emphasized the necessity for greater diversity in leadership positions within higher education. Above all, Robinson and colleagues underscored the imperative of equity and inclusivity in society, advocating that acknowledging the absence of equity can catalyze cultural transformation and encourage inclusiveness.
Barbara Applebaum (2019) focuses instead on institutional culture transformation, finding that if taken in isolation implicit bias trainings are not a panacea. She critically assessed the effectiveness of implicit bias training as a means to drive institutional culture transformation within college campuses. The author contended that although implicit bias training is commonly employed as a response to address racism, sexism, homophobia, and other forms of oppression, it is not without its limitations. Applebaum acknowledged the capacity of implicit bias training in effectively raising awareness about unconscious biases. However, she also raised a critique by pointing out training initiatives’ neglect of the structural and systemic factors that perpetuate oppression within the college environment, which may hinder the essential shifts required for transforming the institutional culture in college campuses.
By examining these diverse studies published in 2019, we garner a more nuanced understanding of how implicit bias operates across different educational contexts, ranging from preschools’ early racial categorizations to higher education’s barriers for women of color and systemic inequalities in special education. The findings and discussions from this section signified an urgent need for multifaceted interventions to disrupt the deeply ingrained biases that perpetuate educational inequities across various age groups and settings. They also underscore the need for attention to the role of implicit bias in the earliest stages of education and resonated with McCardle and Bliss (2019)’s call for investments in our children.
Implicit Bias in Education: 2020
Implicit Bias in Education: 2020We examined twelve (12) articles published in 2020 that investigated the role of implicit racial bias in educational settings. A number of studies published in 2020 further explored the extent of teachers’ implicit racial bias and its influence on their evaluation of students. Prior literature has documented the links between racial biases held by teachers and racial inequality in education outcomes (Warikoo et al., 2016). 2020 research has revealed that it is possible that even well-intentioned teachers may be unconsciously influenced by their implicit biases, which hinder them from promoting racial equity (Starck et al., 2020).
Starck and colleagues (2020) compared teachers’ implicit bias against those of other adults with similar characteristics using two national datasets. The study found that both teachers and nonteachers have similar levels of pro-White implicit racial bias, indicating that teachers’ racial attitudes largely mirror those held by the broader society. Additionally, Chin and colleagues (2020) found that teachers’ implicit biases across the nation varied by teacher gender and race. Female teachers appeared slightly less biased than non-female teachers, and teachers of color appeared to be less biased than White teachers. Overall, teachers’ adjusted bias levels were lower in counties with higher shares of Black students, echoing the role of contextual factors. When the data were analyzed at an aggregated level, counties with higher levels of implicit racial bias among teachers tended to exhibit more pronounced disparities between Black and White students in both test scores and suspension rates. This finding persists even after adjusting for a broad array of covariates at the county level. Together, these two studies showed that schools and the teachers embedded in them should not be considered as separate entities inherently capable of counteracting societal inequalities independently (Starck, 2020)
Furthermore, Quinn (2020) conducted experimental studies to assess the impact of implicit bias on teachers’ evaluations of student writing. On average, teachers showed a significant implicit association between White students and higher writing competency (Quinn, 2020). Racial bias against Black students was found when teachers scored student writing using vague rubrics. Importantly from a mitigation perspective, racial bias was not found when teachers adhered to rubrics with clearer evaluation criteria. These findings lent support to previous implicit bias research on the relationship of evaluation criteria and teacher’s racial bias (Payne & Vuletich, 2018). Quinn (2020) noted that further research should be conducted to determine the influence of bias on specific academic subjects and the nature of the student work being evaluated.
Controlling for explicit racial bias, Marcucci (2020) conducted a survey with racial priming to examine the potential impact of implicit bias on teachers’ disciplinary decision-making. The participating teachers were randomly assigned to either the African American or White condition for the vignette, which served as the racial prime. Subsequently, the teachers were presented with questions regarding their hypothetical responses to the student described in the vignette, specifically addressing disciplinary choices that encompass punitive or rehabilitative approaches. The results indicated that teachers’ implicit bias had a greater impact on punitive disciplinary decisions than on rehabilitative decisions. Counterintuitive to conventional knowledge about anti-Black implicit bias and racial inequalities in discipline, Marcucci (2020) found that teachers treated White students more harshly by making more punitive disciplinary decisions. The author cautioned against interpreting such a finding as evidence for the presence of anti-White implicit bias. Instead, Marcucci (2020) suggested that social desirability might exert a powerful influence on teachers’ decision-making processes in specific contexts. The findings indicated that teachers have the capacity to override anti-Black implicit biases when they are aware of the socially desirable quality for racial neutrality in a reflective setting such as a survey, as opposed to the pressure of a real-time disciplinary interaction. While this overriding tendency may lead to over-correcting standards for White students and lowering expectations for Black students in a harmful manner, it also demonstrated that teachers may be open to engaging in transformative de-biasing strategies. To achieve success in implicit bias mitigation, Marcucci (2020) emphasized the need of restructuring the teaching profession to reduce the cognitive and emotional stress burden on teachers and, consequently, prioritize opportunities for self-reflection.
One recent study investigated the impact of school administrators’ implicit biases on the severity of disciplinary actions (Gullo & Beachum., 2020). With a survey sample of 43 administrators from 22 schools in 7 Pennsylvania school districts, the researchers found that the administrators showed an overall pro-White preference on the Implicit Association Test for race. Discipline data at the individual student-level, including information such as student race, infraction type, disciplinary action, and the deciding administrator for the infraction, was collected from participating districts and schools. It was found that approximately 25% of the differences in discipline severity were based on student race. Most interestingly, the severity of subjective disciplinary decisions, which are not dictated by law, policy, or code, was influenced by administrators’ implicit bias. On the other hand, some of the variations in objective disciplinary decisions were attributed to student race (Gullo & Beachum, 2020). This study is one of the first to demonstrate the influence of administrators’ implicit bias on their subjective discipline decisions.
Taking the findings from Marcucci (2020) and Gullo and Beachum (2020) together, it prompts scholars to consider the multifaceted ways implicit bias manifests itself, showing that it might differ depending on the settings where educational disciplinary practices occur. Marcucci’s controlled, survey setting demonstrated that educators are able to override their implicit biases, leading to unexpected outcomes such as more punitive measures against White students. Marcucci attributed such overriding not to anti-White bias but to the influence of social desirability and a potential over-correction upon reflection. In contrast, Gullo & Beachum’s investigation into real-world disciplinary actions confirmed the persistent effect of implicit biases. Their findings showed a pro-White preference among administrators, indicating that a notable proportion of disciplinary disparity can be attributed to implicit racial bias, particularly in subjective decision-making. These findings collectively emphasize the complexity of implicit bias in educational disciplines, particularly how it impacts punitive versus rehabilitative decisions and objective versus subjective decisions. Please see the Mitigation Section for the authors’ recommended solutions.
In summary, the research from 2020 underlined the varying influence of implicit bias across different levels of educators, not just among teachers who interact with students on a daily basis, but also among school administrators who have power to enforce discipline policies or promote applicable changes to them. In our review, we have uncovered divergent ways of how implicit bias influences educators across different contexts. A highlight that stood out is the nuanced impact implicit bias could have on disciplinary practices. It is crucial to recognize that in environments where educators are conscious of scrutiny, the effect of their implicit racial bias could lead to an overcompensation in disciplinary standards for students from different racial backgrounds. On the other hand, in situations where social desirability is not of concern, implicit bias continues to be associated with disparate subjective disciplinary decisions, leading to unjust treatment of certain student populations. While teachers and administrators may have every good intention to support all students equally, their behaviors and judgments are influenced by both their own implicit bias and deeply embedded systemic biases. These findings come at a crucial time, especially considering the anticipated demographic shift in U.S. schools where the number of racial and ethnic minority students are expected to surpass that of their non-minority peers (Federal Interagency Forum on Child and Family Statistics, 2017).
Mitigating Bias in Education
Mitigating Bias in EducationStudies from 2018-2020 did not simply continue to confirm the last ten or more years of evidence, supporting a direct link between implicit racial bias and educational policies and outcomes. Many studies also proposed and/or tested mitigation strategies, which has led to a crucial debate: Should the focus be on fixing the implicit bias held by students and teachers through awareness training, or should efforts be concentrated at the policy level? Girvan and colleagues (2017) found evidence for the former, showing that when explicit guidelines are provided, individuals are more likely to make equitable decisions. However, just making each individual accountable for their biased decisions isn’t enough. Anyon and colleagues (2018) argued for the necessity of examining specific school settings as a more systemic factor that creates discrepancies in discipline. Their study showed that it is the classroom environment itself that contributes most substantially to the disciplinary disparity among students of color. Furthermore, Tate and Page (2018) raised critiques about individual level implicit bias training. They argued that we must recognize that biases are often interlinked with broader institutional and systemic structures, emphasizing the unconscious nature of implicit bias may downplay the role of White supremacy in maintaining racism. Arlo Kempf (2020) also pointed out that the implicit bias perspective may provide a corporate-friendly lens for understanding racism at the individual level, but it is not enough for disrupting racism at the institutional and structural levels. He called for the use of critical race theory and critical pedagogy as tools to deepen implicit bias intervention approaches.
Heidi Vuletich and Keith Payne (2019) highlights the importance of considering the impact of systemic factors, such as campus-specific social indicators and faculty diversity, on the stability of individual implicit biases. They delved into the critical question of whether implicit bias can be mitigated in the long-term, and if so, under what conditions. Bearing these questions in mind, they revisited a prior study which indicated that although interventions altered participants’ bias immediately after, the effects were not sustained over time (Lai et al., 2016, Study 2). To investigate whether the stability observed in implicit bias reflected persistent individual attitudes or stable environments on campus, Vuletich and Payne reanalyzed the data collected across 18 university sites by Lai and colleagues and identified three measures capturing historical and present inequalities that could potentially influence university community members today. The three measures are: 1) public display of structural inequality (evaluating whether Confederate monuments were displayed on campuses), 2) faculty diversity (a measure reflecting underrepresentation of minority faculty as a signal of institutional inequalities), and 3) campus-specific social mobility (derived from a study estimating social mobility in U.S. universities). Lai and colleagues had previously interpreted the short-lived effects of their interventions as showing that individual’s implicit biases are difficult to change. However, Vuletich and Payne’s further analyses found that the stability of individual implicit biases should be attributed to campus environments reflecting historical and present inequalities. This reinterpretation has important implications for combating discrimination as it suggests that altering the social environment may be more effective than attempting to change individual attitudes. The findings also suggested that eliminating environmental cues of inequality, like Confederate monuments, could potentially reduce overall implicit bias. Similarly, enhancing faculty diversity at universities or diversifying leadership roles within organizations may lead to sustained institutional bias changes.
As we did in the introduction, we classified mitigation strategies into three categories: students, educators, and systems. Table 1 below presents a summary of the mitigation strategies derived from our review of the implicit bias intervention literature, specifically focusing on education published between 2018 and 2020. Each strategy is hyperlinked to facilitate easier navigation for reader.
Mitigation Strategies for Students’ Implicit Biases | |
Davis (2020); | |
Behm-Morawitz &Villamil (2019); | |
Mitigating Implicit Bias Among Educators | |
Provide Voluntary Professional Development Workshops to Educators | Aguilar (2019); |
Holroyd & Saul, 2018; | |
Systemic and Policy-Oriented Mitigation Strategies | |
Gullo & Beachum’s (2020); | |
Clark-Louque & Sullivan (2020); | |
Applebaum (2019); | |
Mitigation Strategies for Students’ Implicit Biases
1. Leverage the Critical Window of Early Childhood Education
Several studies suggest that early education presents a crucial window for addressing implicit bias, including five studies from our samples: two studies by Qian et al., 2019a and 2019b; Setoh et al., 2019; McCardle and Bliss, 2019; and Davis, 2020. The first study by Qian et al. (2019a) found that implicit racial bias against outgroup members was evident in Chinese participants as young as four years old and that implicit anti-Black bias remained stable across the age range from 4 to 19 years old. This finding underscored that implicit racial bias develops at a young age. Returning to Setoh and colleagues’ 2019 study, which recommended that future research should delve into the role of social experiences in shaping children’s understanding of racial categories, the authors proposed a perceptual training approach aimed at reducing children’s automatic inclination to categorize faces based on race, potentially fostering better interracial reactions. Qian et al.’s second study (2019b) did exactly that by shedding light on the development of face-related social processing. This study also offers practical strategies for mitigating implicit racial bias in young children.
Qian and colleagues (2019b) assessed the long-term impact of perceptual individuation training on reducing implicit racial bias in preschool children. The study tracked 95 Chinese preschool children across a period of 70 days. Two perceptual individuation trainings, one initial and one supplementary, were carried out to teach preschoolers to focus on distinctive facial features rather than relying on stereotypes or group attributes. Implicit racial bias was measured at five time points, including before and immediately after each training, as well as 9, 10, and 70 days after the pretest. Results revealed that perceptual individuation training effectively reduced implicit racial bias in preschool children. Specifically, this bias reduction was observed both immediately after the initial training and 70 days after the pretest. These practical approaches could be integrated into school curriculum or utilized by social workers, as suggested by McCardle and Bliss (2019), to address individual factors leading to segregation in the society.
Furthermore, in the wake of the tragic events involving George Floyd, Breonna Taylor, and Ahmaud Arbery, Thamara Davis (2020) discussed the importance of addressing diversity, fair treatment, implicit bias, and racial trauma, particularly in the context of educating young children. She argued that such news events can emotionally impact children, potentially leading to chronic stress, similar to their effects on adults. On the other hand, these events also offer opportunities to teach about privilege, racism and implicit bias. The articles we reviewed documented that children as young as four years old have exhibited implicit racial bias against outgroup members. Therefore, avoiding these topics during this critical window may have unintended consequences. Avoiding discussions on these topics, even with young children, might foster the misconception that race is a taboo topic or create a space where prejudice and bias develop. Davis contended that parents, educators and healthcare professionals should all play a role in holding discussions about implicit bias, as well as the trauma and anxiety surrounding racial violence.
2. Embrace Multicultural Education
A second mitigation strategy we identified in our review of all 33 publications between 2018 to 2020 is an embrace of multicultural education. Multiculturalism can be described as a social and intellectual movement that upholds diversity as a fundamental principle and advocates for the equitable treatment and respect of all cultural groups (APA, 2017). This approach encompasses the incorporation of educational materials and activities designed to foster multicultural awareness, such as diversity quizzes and videos on cultural sensitivity. Three studies from our sample concurred with this strategy.
Behm-Morawitz and Villamil (2019) turned our attention to the digital realm and investigated the effectiveness of innovative online diversity training in higher education. Specifically, the research examines how an online program impacts undergraduate students’ attitudes toward diversity, motivation to control prejudice, and bias reduction toward African Americans. The study discussed a comprehensive approach to assessing bias, employing both direct (self-report) and indirect measures. With the indirect measure of the Implicit Association Test (IAT) to gauge implicit bias against African Americans, the results revealed that completing the online diversity program led to decreased implicit bias and enhanced openness to diversity. Furthermore, the researchers found that lessons addressing identity, stereotyping, housing discrimination, and education discrimination are particularly effective in engaging students with intergroup-based diversity instruction. Additionally, Behm-Morawitz and Villamil noted that the classroom setting is susceptible to society’s evolving and diverse worldviews. Therefore, when drafting online diversity training programs, it is crucial to consider the polarized U.S. political climate and students’ diverse perspectives, employing strategies such as interactive language and a second person viewpoint to draw viewers into a deeper engagement with the materials being presented. McCardle and Bliss (2019) expanded on this conversation by suggesting school integration can be seen as a strategy to promote multiculturalism as well. Their study observed a direct correlation between perceived diverse experiences and reduced implicit bias. This finding indicated that school integration could provide students with more diverse life experiences, which would better equip students’ adult life in a multiracial society by allowing more opportunities to have genuine interactions with people from different racial, regional, and socioeconomic backgrounds.
Black and Li (2020) based their research on previous culture-related studies and hypothesized that cultivating multiculturalism can be a possible solution to mitigating intergroup bias problems. For instance, trainings that emphasized cultural awareness and diversity issues were found to be a useful tool for the on-the-job education of healthcare professionals to improve cultural competency (Smith, 1998), self-awareness of cultural bias (Carter et al., 2006), and reduce stigmatization (Hayes et al., 2004). Such training programs were shown to be effective on both educators and students of different ages in improving attitude to and social engagement with outgroup members of different races and ethnicities (Turner & Brown, 2008; Warring et al., 1998; Sakurai et al., 2010). In the context of this study, intervention techniques were employed to familiarize participants with educational materials centered around multiculturalism. Black and Li’s 2020 experimental study involved random assignment of 249 undergraduate students to intervention or control conditions and found that their virtual intervention strategies successfully increased multiculturalism scores among undergraduate students. Five major sets of activities were contained in the educational materials, including a diversity awareness quiz, “My Multicultural self”; cultural sensitivity scenarios; microaggression-related educational videos, cultural appropriation, and implicit bias; and scenarios illustrating advocacy and taking proactive measures against racism. The authors argued that multiculturalism may positively influence implicit and explicit cultural attitudes, perceptions, and behaviors. This positive result of intervention demonstrates the possibility of using inexpensive and time-efficient methods to address biases in student populations.
Mitigating Implicit Bias Among Educators
1. Voluntary Professional Development Workshops:
One of the more traditional ways of mitigating implicit bias at individual level is through workshops and training programs for teachers to raise awareness about implicit bias and offer tools for introspection and self-improvement. Equipping educators with the tools they need to combat implicit bias and foster equitable educational environments is a crucial tool for disrupting the harms students of color often face due to implicit racial bias in the classroom. Our review identified four (4) studies over the three-year period that focused specifically on professional development training for educators.
Educators may not consciously endorse stereotypes, but implicit racial bias is sufficient to make an individual quickly perceive youth of color, particularly males, as threatening and justify punitive measures against them (Brown, 2018; Eberhardt et al., 2004; Mendez et al., 2002; Skiba et al., 2011; Wallace et al., 2008). Therefore, it is crucial for educators to disrupt the perpetuation of dysfunctional educational ecologies by learning and understanding the racial discourses that inform implicit bias in schools (Annamma & Morrison, 2018). Aguilar (2019) explored the potential impact of mindfulness and awareness cultivation on educators’ ability to recognize and disrupt unconscious biases, leading to a reduction in opportunity gaps within educational institutions. Aguilar (2019) emphasized the importance of acknowledging the concept of race as a detrimental narrative that perpetuates inequities in education, including the belief that students from specific backgrounds possess diminished capabilities or that certain student groups are predisposed to behavioral issues. These narratives can foster implicit biases that impact educators’ interactions and support for students, thus contributing to the persistence of opportunity gaps. To address this issue, Aguilar (2019) provided an illustrative example of a mindfulness professional development session implemented in school, as a result of this session, educators were able to proactively intercept racist thoughts as they arise, enabling them to consciously choose their responses and actions.
In their study of women of color students and faculty, Robinson et al. (2019) proposed remedies such as creating new courses centered on diversity and inclusivity, establishing safe spaces for discussions on race and sensitive topics, involving faculty in sensitivity training, and forming affinity groups to address the needs of students of color. Additionally, drawing from a previous study (Jackson et al., 2014), Robinson et al. reiterated the effectiveness of diversity training in reducing stereotypes in STEM fields and fostering a more inclusive environment. Robinson and colleagues concluded that educational institutions should prioritize support programs involving mentoring to effectively recruit and retain diverse students and faculty.
Harrison-Bernard and colleagues (2020) documented the processes and results of a professional development workshop on implicit bias held at a university. The six workshops consisted of various didactic teaching modules, active participation, and discussions aimed at increasing participants’ introspection and implicit bias awareness. Pre- and post-workshop surveys were conducted to assess participants’ self-perception of knowledge and behaviors related to diversity and implicit bias. The surveys showed that participants’ knowledge of implicit bias increased significantly as a result of the workshops. Moreover, an observational study of a single 90-minute racial affinity caucusing workshop was also conducted to for educators interested in racial health disparities (Guh et al., 2020). The workshop successfully improved participants’ impression of and confidence in implementing racial affinity caucusing. Both studies effectively demonstrate that educators’ knowledge and attitudes regarding implicit bias intervention tools can be changed even in a much shorter period of time. These studies called attention to the need for effective tools to teach and remedy the impact of implicit racial bias in education.
2. Foster Empathy and Equal Expectations for All Students
Empathy-based intervention has been using in various areas of study, such as teacher-student interaction (Okonofua et al., 2016) and healthcare-related education (Batt-Rawden et al., 2013; McGuire, 2016). Research findings exemplified by the Whitford and Emerson (2019) study showcased the potential of empathy interventions to mitigate implicit bias among pre-service teachers. The authors conducted an experiment to examine whether a brief empathy-inducing intervention could reduce implicit bias among pre-service teachers who planned to work in elementary schools. This intervention required participants to read 10 instances of racism that Black students encountered. Subsequently, participants were asked to put themselves in the students' situations, express their feelings about the experiences, detail how they would react in those scenarios, describe the potential emotions of growing up in such an environment, and suggest ways to prevent similar experiences in the future. The results showed that the empathy intervention significantly decreased implicit bias among White female pre-service teachers towards Black individuals. School discipline disparities contribute to the prison pipeline for at-risk students (Skiba et al., 2014). Empathy intervention conducted in Whitford and Emerson could serve as a foundation for promoting change and addressing implicit bias in education.
In addition to the cultivation of empathy, another similar theme also surfaced from our synthesis, underscoring the imperative of fostering equal consideration for students from diverse backgrounds. Researchers have urged educators to maintain high expectations for all students, while also being vigilant about the harmful effects of stereotype threats. This is particularly crucial for fields such as STEM education and philosophy, where minority students are severely underrepresented (Haring-Smith, 2012; Holroyd & Saul, 2018; Farrell & Minerick, 2018). In their 2018 study on chemical engineering education, Farrell and Minerick drew our attention to the fact that, due to implicit biases, educators often direct their time and resources toward students they deem most likely to be successful. To combat these challenges, the authors suggested that both students and educators have responsibilities in addressing them. Students should strive to be more mature and adaptive problem-solvers, while of course fulfilling class requirements to the best of their abilities., Educators should employ as objective a grading system as possible. Furthermore, educators should acknowledge their implicit biases, pursue self-education regarding these biases, and remain cognizant of stereotype threat and its negative impacts on students. Educators also need to send consistent messages of high expectations and anticipated success to all students in the class. Importantly, educators should not perceive limited prior experience and low confidence in engineering as deficits as these are common traits for students from underrepresented groups in engineering. Instead, these characteristics should be considered as indicators of assets that may aid students in their journey to becoming engineers.
Systemic and Policy-Oriented Mitigation Strategies
1. Utilize Objective Decision-Making Standards
The objective decision-making standards approach involves the application of data-driven methodologies and explicit guidelines to identify, analyze, and address disciplinary disparities. McIntosh and colleagues (2018) deepened scholars’ engagement with the approach by testing a four-step, data-driven decision-making strategy. This method helps to identify the interactions that are susceptible to implicit bias and then tailors the environment to meet all students' needs. The first step, problem identification, involves calculating disproportionality metrics by incorporating both risk ratios and absolute rates by subgroups. The metrics will establish the baseline for monitoring progress. Next, during the problem analysis step, potential causes for the disproportionality are identified. Tools such as the School-Wide Information System (SWIS) are recommended for examination of discipline patterns such as location, time of day, and type of behavior by subgroup. The third step is plan implementation, in which existing systems are evaluated and potentially revised to better meet student needs. McIntosh et al. (2018) recommended a flexible, proactive, multi-tiered behavioral approach that incorporates explicit expectations and accommodates the needs of students, families, and the community. This approach also promotes objective discipline procedures, such as clearly defining problematic behaviors. Finally, in the plan evaluation step, the implementation of the plan is assessed through established measures, and the original disproportionality metrics are recalculated. These are then compared with the initially identified equity goals. In a case study using this approach, McIntosh et al. (2018) noted a consistent decrease in discipline disproportionality, reinforcing the effectiveness of this objective, data-driven strategy. Gullo and Beachum's 2020 study also highlighted the importance of having clear and objective policy guidelines and procedures to help reduce the racial discipline. They also emphasized the need for schools to make efforts to expand objective policies and remove the subjective nature of many disciplinary decisions when possible.
2. Replace Negative Impact Policies with Restorative Measures
Much of the research at the systemic level has focused on the alarming disparities in K-12 school discipline. School discipline disparities contribute to the school-to-prison pipeline for marginalized students (Skiba et al., 2014). Existing policies in the current education system sometimes inadvertently contribute to the disproportionately high rates of disciplinary actions against marginalized student populations. Zero Tolerance policies are one of them (Clark-Louque & Sullivan, 2020). Zero Tolerance was originally developed and introduced to public schools in an effort to make schools safer. It operates under two basic assumptions: 1) harsh disciplines will deter student misconduct, and 2) removal of students who committed the most serious offenses will benefit the school. However, these assumptions are problematic as school principals’ attitudes are subjective and can be influenced by implicit racial bias. Recently, Zero Tolerance policies have expanded to include relatively minor issues such as dress code violations, disrespect, and willful defiance, which were observed among the common infractions leading to suspension. Notably, disrespect and willful defiance are subjective concepts which, when applied, are rife with the risk of implicit racial bias influence due to their vagueness – everyone has their own understanding of respect and defiance (Girvan et al., 2017; Skiba et al., 2002; 2011). Excessive reliance on punitive forms of discipline such as suspension was directly linked to students’ tendencies to drop out of school susceptibility to being ensnared by the criminal justice system (Fergus, 2015).
At the school administration level, Clark-Louque and Sullivan (2020) discussed the disproportionate discipline consequences faced by Black girls and linked it to the implicit biases held by some school officials. They argued that these biases, which are based on stereotypes that see Black women and girls as hypersexual, sassy, conniving, or loud (Morris, 2016), distort the views of school officials towards Black girls and resulted in the disciplinary actions taken based on Zero Tolerance policies. Clark-Louque and Sullivan (2020) presented two real-life scenarios in which Black female students were suspected of using marijuana. In one scenario, the school administration followed a Zero Tolerance approach, while in the second scenario the administration adopted a restorative and equity-based partnering approach such as asking questions that allow students to express themselves and inviting students to sign up for counseling. Under the first scenario, the student involved was eventually expelled. The four students involved in the second scenario, however, were given an opportunity to meet with the school counselor and their families were notified regarding safety concerns and future possible engagement strategies. Based on their findings the researchers strongly recommended that school administrators should guard against implicit and explicit biases by adopting restorative practices and build culturally proficient partnerships with student families instead of relying heavily on Zero Tolerance practices.
Furthermore, Romero and colleagues (2020) reviewed a number of promising studies that may shed light on how to alleviate implicit bias in school discipline. Their review showed that less punitive alternatives such as restorative justice, as opposed to the Zero Tolerance approach, are gaining popularity in schools. Romero and colleagues recommended training and intervention strategies to educators, including empathetic mindset training, motivated self-regulation, and prejudice habit-breaking interventions. The researchers emphasized that mitigating implicit bias in schools requires a sustained approach that raises awareness of implicit bias and its consequences in educational settings. This calls for the inclusion of individual level implicit bias assessments coupled with careful feedback on the results and sustained professional development.
Marcucci (2020) also championed restorative measures. Her study found that implicit bias appeared to have less influence on rehabilitative disciplinary decisions compared to punitive ones. According to Marcucci (2020), restorative practices are able to compel students and educators to find novel ways of interaction, which may humanize the students and allow educators to reflect and disrupt automatic and unconscious biased thinking. Echoing Marcucci (2020)’s findings, McIntosh and colleagues further underscored this perspective with their flexible four-step behavioral approach that exemplified the restorative measures. By pinpointing “physical aggression on the playground” as a specific vulnerable decision point that increases the likelihood of implicit bias affecting discipline decision making, the research team advised educators to set clear expectations and meet the needs of students, families, and the community. This restorative approach fosters objective discipline procedures, which have resulted in a consistent decrease in disciplinary disparity over time.
3. Utilize a Holistic Approach
The first two systemic mitigation strategies lead us to a third and final strategy: using a holistic approach. By this we mean crafting approaches that include but are not limited to mitigating implicit racial bias. This approach complements individual-level interventions by addressing the broader environmental factors that contribute to implicit bias, suggesting that sustained change may require a comprehensive strategy that includes altering the social environment.
Applebaum’s critical read of implicit bias trainings is one example. In lieu of an exclusive reliance on implicit bias training, Applebaum advocated for a more comprehensive and holistic approach that attends to systemic as well as individual and intergroup factors. Another example is proposed by Rynders (2019), who provided possible legal solutions that lawyers can employ in the courtroom and within their own practice to address implicit bias. These solutions include using expert witnesses to testify about implicit bias, using data to show disproportionality, and advocating for culturally responsive teaching practices. At the end of his discussion, Rynders called for educators and advocates to acknowledge the impact of implicit bias in these disparities and integrate research-based approaches to mitigate racial biases. He also emphasized the role of attorneys in education, asserting that special education lawyers should address racial and national origin discrimination as necessary and partner with racial justice organizations to attain educational equity.
In a similar vein, Holroyd and Saul (2018) widened the discussion to include faculty hiring and professional development. They emphasized the need for proactive strategies to counter these biases in decision-making and interactions. To specifically address the entrenched issue of implicit bias in philosophy, they offered various reform suggestions, including: diversifying the subject matter taught, setting hiring criteria in advance, and reducing dependence on letters of recommendation as a key element in faculty selection.
In response to racially disproportionate expulsion rates in preschools (Meek & Gilliam, 2016), Davis and colleagues (2020) take a more systemic approach to combating implicit bias in early education. Their theoretical framework, the Infant and Early Childhood Mental Health Consultation (IECMHC), can reduce the influence of implicit bias on educators’/teachers’ disciplinary decisions. IECMHC was developed to account for the roles played by mental health consultants in building teachers’ capacities to support the healthy social-emotional development of young children. The framework underlined the power of a strong consultative alliance between teachers and consultants with expertise in infant and early childhood mental health. This consultative alliance can be built through multiple core tasks, including: asking reflective questions, creating a holding environment for others’ emotions, raising issues of race and gender, cultivating cultural awareness, and exploring contextual influences such as parenting, trauma, cultural expectations, and developmental differences. A strong consultative alliance, in turn, can contribute to increases in reflective capacity and changes in teachers’ perspective and behavior, both of which are expected to reduce the influence of implicit bias on expulsion rates. In addition to professional help, facilitated workshops for teachers and staff members have also been created and implemented.
Building on the aforementioned strategies, the final mitigation strategy we have identified focuses on transforming the campus environment as a whole. As we noted earlier, Vuletich and Payne’s (2019) findings offered us a roadmap for this transformative approach. Their findings emphasized the power of environmental cues on campus, such as Confederate monuments and level of faculty diversity, in perpetuating biases. By addressing these historical and present inequalities embedded within the campus environment, universities have the potential to significantly reduce implicit bias.
References
ReferencesReferences
Aguilar, E. (2019). Getting mindful about race in schools. Educational Leadership, 76(7), 62-67.
American Psychological Association. (2017). Multicultural guidelines: An ecological approach to context, identity, and intersectionality. http://www.apa.org/about/policy/multicultural-guidelines.aspx
Annamma, S., & Morrison, D. (2018). Identifying dysfunctional education ecologies: A DisCrit analysis of bias in the classroom. Equity & Excellence in Education, 51(2), 114-131. https://doi.org/10.1080/10665684.2018.1496047
Anyon, Y., Lechuga, C., Ortega, D., Downing, B., Greer, E., & Simmons, J. (2018). An exploration of the relationships between student racial background and the school sub-contexts of office discipline referrals: A critical race theory analysis. Race Ethnicity and Education, 21(3), 390-406. https://doi.org/10.1080/13613324.2017.1328594
Applebaum, B. (2019). Remediating campus climate: Implicit bias training is not enough. Studies in Philosophy and Education, 38, 129-141. https://doi.org/10.1007/s11217-018-9644-1
Aud, S., KewalRamani, A., & Frohlich, L. (2011). America’s youth: Transitions to adulthood (NCES 2012-026). National Center for Education Statistics. https://files.eric.ed.gov/fulltext/ED527636.pdf
Banks J. A., Cochran-Smith M., Moll L., Richert A., Zeichner K., LePage P., Darling-Hammond L., Duffy H., McDonald M. (2005). Teaching diverse learners. In Darling-Hammond L., Bransford J. (Eds.), Preparing teachers for a changing world: What teachers should learn and be able to do (pp. 232–274). Jossey-Bass.
Batt-Rawden, S. A., Chisolm, M. S., Anton, B., & Flickinger, T. E. (2013). Teaching empathy to medical students: An updated, systematic review. Academic Medicine, 88(8), 1171–1177. https://doi.org/10.1097/ACM.0b013e318299f3e3
Behm-Morawitz, E., & Villamil, A. M. (2019). The roles of ingroup identification and implicit bias in assessing the effectiveness of an online diversity education program. Journal of Applied Communication Research, 47(5), 505-526. https://doi.org/10.1080/00909882.2019.1678761
Black, K., & Li, M. (2020). Developing a virtual multicultural intervention for university students. Behavioral Sciences, 10(11), 186-209. https://doi.org/10.1080/01608061.2020.1832014
Botts, T. F., Bright, L. K., Cherry, M., Mallarangeng, G., & Spencer, Q. (2014). What is the state of blacks in philosophy?. Critical Philosophy of Race, 2(2), 224-242. https://doi.org/10.5325/critphilrace.2.2.0224
Brown, A. (2018). From subhuman to human kind: Implicit bias, racial memory, and black males in schools and society. Peabody Journal of Education, 93(1), 52-65. https://doi.org/10.1080/0161956X.2017.1403176
Carter, M. M., Lewis, E. L., Sbrocco, T., Tanenbaum, R., Oswald, J. C., Sykora, W., Williams, P., & Hill, L. D. (2006). Cultural competency training for third-year clerkship students: Effects of an interactive workshop on student attitudes. Journal of the National Medical Association, 98(11), 1772–1778.
Chin, M. J., Quinn, D. M., Dhaliwal, T. K., & Lovison, V. S. (2020). Bias in the air: A nationwide exploration of teachers’ implicit racial attitudes, aggregate bias, and student outcomes. Educational Researcher, 49(8), 566–578.https://doi.org/10.3102/0013189X20937240
Clark-Louque, A., & Sullivan, T. A. (2020). Black girls and school discipline: Shifting from the narrow zone of zero tolerance to a wide region of restorative practices and culturally proficient partnerships. Journal of Leadership, Equity, and Research, 6, Article 2.
Correll, J., Park, B., Judd, C. M., & Wittenbrink, B. (2002). The police officer's dilemma: Using ethnicity to disambiguate potentially threatening individuals. Journal of Personality and Social Psychology, 83(6), 1314–1329.
Davis, A. E., Perry, D. F., & Rabinovitz, L. (2020). Expulsion prevention: Framework for the role of infant and early childhood mental health consultation in addressing implicit biases. Infant Mental Health Journal, 41(3), 327-339. https://doi.org/10.1002/imhj.21847
Davis, L. (2013). Introduction: Disability, normality and power. In Lennard J Davis (Ed.), The disability studies reader (pp. 1-14). Taylor & Francis.
Davis, T. (2020). The role of parents, educators, and treatment providers in educating children about racial injustice. The Brown University Child and Adolescent Behavior Letter, 36(9), 8-8.
Eberhardt, J. L., Goff, P. A., Purdie, V. J., & Davies, P. G. (2004). Seeing Black: Race, crime, and visual processing. Journal of Personality and Social Psychology, 87(6), 876–893. https://doi.org/10.1037/0022-3514.87.6.876
Fabelo, T., Thompson, M. D., Plotkin, M., Carmichael, D., Marchbanks, M. P., III, & Booth, E. A. (2011). Breaking school’s rules: A statewide study of how school discipline relates to students’ success and juvenile justice involvement. Council of State Governments Justice Center; Public Policy Research Institute of Texas A&M University. https://csgjusticecenter.org/wp-content/uploads/2012/08/Breaking_Schools_Rules_Report_Final.pdf
Farrell, S., & Minerick, A. (2018). Perspective: The stealth of implicit bias in chemical engineering education, its threat to diversity, and what professors can do to promote an inclusive future. Chemical Engineering Education, 52(2), 129-135.
Federal Interagency Forum on Child and Family Statistics. (2017). Race and Hispanic origin composition: Percentage of U.S. children ages 0–17 by race and Hispanic origin, 1980–2017 and projected 2018–2050. Forum on Child and Family Statistics. https://www.childstats.gov/americaschildren/tables/pop3.asp
Fergus, E. (2015). A breakthrough on discipline. National Association of Elementary School Principals. https://www.naesp.org/principal-novemberdecember-2015-breaking-cycle/breakthrough-discipline
Forgiarini, M., Gallucci, M., & Maravita, A. (2011). Racism and the empathy for pain on our skin. Frontiers in psychology, 2, Article 108. https://doi.org/10.3389/fpsyg.2011.00108
Gershenson, S., Holt, S. B., & Papageorge, N. W. (2016). Who believes in me? The effect of student–teacher demographic match on teacher expectations. Economics of Education Review, 52, 209-224. https://doi.org/10.1016/j.econedurev.2016.03.002
Gilliam, W. S., Maupin, A. N., & Reyes, C. R. (2016). Early childhood mental health consultation: Results of a statewide random-controlled evaluation. Journal of the American Academy of Child and Adolescent Psychiatry, 55(9), 754–761. https://doi.org/10.1016/j.jaac.2016.06.006
Girvan, E. J., Gion, C., McIntosh, K., & Smolkowski, K. (2017). The relative contribution of subjective office referrals to racial disproportionality in school discipline. School Psychology Quarterly: The Official Journal of the Division of School Psychology, American Psychological Association, 32(3), 392–404. https://doi.org/10.1037/spq0000178
Goff, P. A., Eberhardt, J. L., Williams, M. J., & Jackson, M. C. (2008). Not yet human: Implicit knowledge, historical dehumanization, and contemporary consequences. Journal of Personality and Social Psychology, 94(2), 292–306. https://doi.org/10.1037/0022-3514.94.2.292
Goff, P. A., Jackson, M. C., Di Leone, B. A. L., Culotta, C. M., & DiTomasso, N. A. (2014). The essence of innocence: Consequences of dehumanizing Black children. Journal of Personality and Social Psychology, 106(4), 526–545. https://doi.org/10.1037/a0035663
Guh, J., Krinsky, L., White-Davis, T., Sethi, T., Hayon, R., & Edgoose, J. (2020). Teaching racial affinity caucusing as a tool to learn about racial health inequity through an experiential workshop. Family Medicine, 52(9), 656-660. https://doi.org/10.22454/FamMed.2020.596649
Gullo, G. L., & Beachum, F. D. (2020). Does implicit bias matter at the administrative level? A study of principal implicit bias and the racial discipline severity gap. Teachers College Record, 122(3), 1-28. https://doi.org/10.1177/016146812012200309
Hannon, L., DeFina, R., & Bruch, S. (2013). The relationship between skin tone and school suspension for African Americans. Race and Social Problems, 5(4), 281–295. https://doi.org/10.1007/s12552-013-9104-z
Haring-Smith, T. (2012). Broadening our definition of diversity. Liberal Education, 98(2), 6-13.
Harrison-Bernard, L. M., Augustus-Wallace, A. C., Souza-Smith, F. M., Tsien, F., Casey, G. P., & Gunaldo, T. P. (2020). Knowledge gains in a professional development workshop on diversity, equity, inclusion, and implicit bias in academia. Advances in Physiology Education, 44(3), 286-294. https://doi.org/10.1152/advan.00164.2019
Hayes, S. C., Bissett, R., Roget, N., Padilla, M., Kohlenberg, B. S., Fisher, G., ... & Niccolls, R. (2004). The impact of acceptance and commitment training and multicultural training on the stigmatizing attitudes and professional burnout of substance abuse counselors. Behavior therapy, 35(4), 821-835. https://doi.org/10.1016/S0005-7894(04)80022-4
Holroyd, J., & Saul, J. (2018). Implicit bias and reform efforts in philosophy. Philosophical Topics, 46(2), 71-102.
Houser, C., & Lemmons, K. (2018). Implicit bias in letters of recommendation for an undergraduate research internship. Journal of Further and Higher Education, 42(5), 585-595. https://doi.org/10.1080/0309877X.2017.1301410
Jackson, S. M., Hillard, A. L., & Schneider, T. R. (2014). Using implicit bias training to improve attitudes toward women in STEM. Social Psychology of Education, 17, 419-438. https://doi.org/10.1007/s11218-014-9259-5
Jacoby-Senghor, D. S., Sinclair, S., & Smith, C. T. (2015). When bias binds: Effect of implicit outgroup bias on ingroup affiliation. Journal of Personality and Social Psychology, 109(3), 415–433. https://doi.org/10.1037/a0039513
Kang, S. K., & Bodenhausen, G. V. (2015). Multiple identities in social perception and interaction: Challenges and opportunities. Annual Review of Psychology, 66, 547–574. https://doi.org/10.1146/annurev-psych-010814-015025
Kempf, A. (2020). If we are going to talk about implicit race bias, we need to talk about structural racism: Moving beyond ubiquity and inevitability in teaching and learning about race. Taboo: The Journal of Culture and Education, Special Issue: 50 Years of Critical Pedagogy and We Still Aren’t Critical, 19(2), Article 10.
Kouchaki, M., & Smith, I. H. (2014). The morning morality effect: The influence of time of day on unethical behavior. Psychological Science, 25(1), 95–102. https://doi.org/10.1177/0956797613498099
Kumar, R., Karabenick, S. A., & Burgoon, J. N. (2015). Teachers’ implicit attitudes, explicit beliefs, and the mediating role of respect and cultural responsibility on mastery and performance-focused instructional practices. Journal of Educational Psychology, 107(2), 533–545. https://doi.org/10.1037/a0037471
Ladson-Billings, G. (1994). What we can learn from multicultural education research. Educational leadership, 51(8), 22-26.
Lai, C. K., Skinner, A. L., Cooley, E., Murrar, S., Brauer, M., Devos, T., Calanchini, J., Xiao, Y. J., Pedram, C., Marshburn, C. K., Simon, S., Blanchar, J. C., Joy-Gaba, J. A., Conway, J., Redford, L., Klein, R. A., Roussos, G., Schellhaas, F. M. H., Burns, M., . . . Nosek, B. A. (2016). Reducing implicit racial preferences: II. Intervention effectiveness across time. Journal of Experimental Psychology: General, 145(8), 1001–1016. https://doi.org/10.1037/xge0000179
Logan J. R. (2013). The Persistence of segregation in the 21st century metropolis. City & Community, 12(2), 160-168. https://doi.org/10.1111/cico.12021
Marcucci, O. (2020). Implicit bias in the era of social desirability: Understanding antiblackness in rehabilitative and punitive school discipline. The Urban Review, 52(1), 47-74. https://doi.org/10.1007/s11256-019-00512-7
McCardle, M., & Bliss, S. (2019). Digging deeper: The relationship between school segregation and unconscious racism. Smith College Studies in Social Work, 89(2), 114–131. https://doi.org/10.1080/00377317.2019.1686929
McGee, E. O. (2021). Black, brown, bruised: How racialized STEM education stifles innovation. Harvard Education Press.
McGuire, J. M., Bynum, L. A., & Wright, E. (2016). The effect of an elective psychiatry course on pharmacy student empathy. Currents in Pharmacy Teaching and Learning, 8, 565–571. https://doi.org/10.1016/j.cptl.2016.03.005
McIntosh, K., Ellwood, K., McCall, L., & Girvan, E. J. (2018). Using discipline data to enhance equity in school discipline. Intervention in school and clinic, 53(3), 146-152. https://doi.org/10.1177/1053451217702130
Meek, S.E., & Gilliam, W.S. (2016). Expulsion and suspension in early education as matters of social justice and health equity. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC.
Mendez, L. M. R., Knoff, H. M., & Ferron, J. M. (2002). School demographic variables and out-of-school suspension rates: A quantitative and qualitative analysis of a large, ethnically diverse school district. Psychology in the Schools, 39, 259–277. https://doi.org/10.1002/pits.10020
Morris, M. W. (2016). Pushout: The criminalization of Black girls in school. The New Press.
Navarrete, C. D., McDonald, M. M., Molina, L. E., & Sidanius, J. (2010). Prejudice at the nexus of race and gender: An outgroup male target hypothesis. Journal of Personality and Social Psychology, 98(6), 933–945. https://doi.org/10.1037/a0017931
Nosek B. A., Smyth F. L., Hansen J. J., Devos T., Lindner N. M., Ranganath K. A., Smith C. T., Olson K. R., Chugh D., Greenwald A. G., Banaji M. R. (2007). Pervasiveness and correlates of implicit attitudes and stereotypes. European Review of Social Psychology, 18, 36–88. https://doi.org/10.1080/10463280701489053
Nowicki, J. M. (2018). K-12 Education: Discipline disparities for Black students, boys, and students with disabilities (GAO-18-258). U.S. Government Accountability Office. https://files.eric.ed.gov/fulltext/ED590845.pdf
Oelrich, N. M. (2012). New idea: Ending racial disparity in the identification of students with emotional disturbance. South Dakota Law Review, 57(1), 9-41.
Okonofua, J. A., & Eberhardt, J. L. (2015). Two strikes: Race and the disciplining of young students. Psychological Science, 26(5), 617–624. https://doi.org/10.1177/0956797615570365
Okonofua, J. A., Paunesku, D., & Walton, G. M. (2016). Brief intervention to encourage empathic discipline cuts suspension rates in half among adolescents. Proceedings of the National Academy of Sciences of the United States of America, 113(19), 5221–5226. https://doi.org/10.1073/pnas.1523698113
Parekh, G., Brown, R. S., & Zheng, S. (2018). Learning skills, system equity, and implicit bias within Ontario, Canada. Educational Policy, 35(3), 395–421. https://doi.org/10.1177/0895904818813303
Payne, B. K., & Vuletich, H. A. (2018). Policy insights from advances in implicit bias research. Policy Insights from the Behavioral and Brain Sciences, 5(1), 49-56. https://doi.org/10.1177/2372732217746190
Perszyk, D. R., Lei, R. F., Bodenhausen, G. V., Richeson, J. A., & Waxman, S. R. (2019). Bias at the intersection of race and gender: Evidence from preschool‐aged children. Developmental Science, 22(3), 1–8. https://doi.org/10.1111/desc.12788
Purdie-Vaughns, V., & Eibach, R. P. (2008). Intersectional invisibility: The distinctive advantages and disadvantages of multiple subordinate-group identities. Sex Roles: A Journal of Research, 59(5-6), 377–391. https://doi.org/10.1007/s11199-008-9424-4
Qian, M. K., Heyman, G. D., Quinn, P. C., Fu, G., & Lee, K. (2019a). Differential developmental courses of implicit and explicit biases for different other-race classes. Developmental Psychology, 55(7), 1440-1452. https://dx.doi.org/10.1037/dev0000730
Qian, M. K., Quinn, P. C., Heyman, G. D., Pascalis, O., Fu, G., & Lee, K. (2019b). A long‐term effect of perceptual individuation training on reducing implicit racial bias in preschool children. Child Development, 90(3), e290-e305. https://doi.org/10.1111/cdev.12971
Quinn, D. M. (2020). Experimental evidence on teachers’ racial bias in student evaluation: The Role of grading scales. Educational Evaluation and Policy Analysis, 42(3), 375–392. https://doi.org/10.3102/0162373720932188
Redfield, S. E., & Kraft, T. (2012). What color is special education. Journal of Law & Education, 41(1), 129-200.
Robinson, N. C., Williams-Black, T., Smith, K. V., & Harges, A. (2019). It all started with a picture: Reflections on existing as women of color in a PWI. Multicultural Perspectives, 21(1), 41-52.
Romero, L. S., Scahill, V., & Charles, S. R. (2020). Restorative approaches to discipline and implicit bias: Looking for ways forward. Contemporary School Psychology, 24, 309-317. https://doi.org/10.1007/s40688-020-00314-9
Rothstein, R. (2013). Why children from lower socio-economic classes, on average, have lower academic achievement than middle-class children. In P. Carter & K. Welner (Eds.), Closing the opportunity gap: What Americans must do to give every child an even chance (pp. 61–76). Oxford University Press.
Rynders, D. (2019). Battling implicit bias in the idea to advocate for African American students with disabilities. Touro Law Review, 35(1), 461-480.
Theriot, M. T., & Dupper, D. R. (2010). Student discipline problems and the transition from elementary to middle school. Education and Urban Society, 42(2), 205-222. https://doi.org/10.1177/0013124509349583
Sakurai, T., McCall-Wolf, F., & Kashima, E. S. (2010). Building intercultural links: The impact of a multicultural intervention programme on social ties of international students in Australia. International journal of intercultural relations, 34(2), 176-185. https://doi.org/10.1016/j.ijintrel.2009.11.002
Setoh, P., Lee, K. J. J., Zhang, L., Qian, M. K., Quinn, P. C., Heyman, G. D., & Lee, K. (2019). Racial categorization predicts implicit racial bias in preschool children. Child Development, 90(1), 162–179. https://doi.org/10.1111/cdev.12851
Sidanius, J., & Veniegas, R. C. (2000). Gender and race discrimination: The interactive nature of disadvantage. In S. Oskamp (Ed.), Reducing prejudice and discrimination (pp. 47–69). Lawrence Erlbaum Associates Publishers.
Skiba, R. J., Arredondo, M. I., & Williams, N. T. (2014). More than a metaphor: The contribution of exclusionary discipline to a school-to-prison pipeline. Equity & Excellence in Education, 47(4), 546–564. https://doi.org/10.1080/10665684.2014.958965
Skiba, R. J., Horner, R. H., Chung, C. G., Rausch, M. K., May, S. L., & Tobin, T. (2011). Race is not neutral: A national investigation of African American and Latino disproportionality in school discipline. School Psychology Review, 40(1), 85-107.
Skiba, R. J., Michael, R. S., Nardo, A. C., & Peterson, R. (2002). The color of discipline: Sources of racial and gender disproportionality in school punishment. Urban Review, 34(4), 317–342.
Smith, L. S. (1998). Evaluation of an educational intervention to increase cultural competence among registered nurses [Doctoral dissertation, The University of Alabama at Birmingham]. ProQuest Dissertations & Theses Global.
Staats, C. (2014). State of the science: Implicit bias review 2014. The Kirwan Institute for the Study of Race and Ethnicity.
Staats, C., & Patton, C. (2013). State of the science: Implicit bias review 2013. The Kirwan Institute for the Study of Race and Ethnicity.
Staats, C., Capatosto, K., Tenney, L., & Mamo, S. (2017). State of the science: Implicit bias review 2017. The Kirwan Institute for the Study of Race and Ethnicity.
Staats, C., Capatosto, K., Wright, R. A., & Contractor, D. (2015). State of the science: Implicit bias review 2015. The Kirwan Institute for the Study of Race and Ethnicity.
Staats, C., Capatosto, K., Wright, R. A., & Jackson, V. W. (2016). State of the science: Implicit bias review 2016. The Kirwan Institute for the Study of Race and Ethnicity.
Starck, J. G., Riddle, T., Sinclair, S., & Warikoo, N. (2020). Teachers are people too: Examining the racial bias of teachers compared to other American adults. Educational Researcher, 49(4), 273–284. https://doi.org/10.3102/0013189X20912758
Tate, S. A., & Page, D. (2018). Whiteliness and institutional racism: Hiding behind (un)conscious bias. Ethics and Education, 13(1), 141-155. https://doi.org/10.1080/17449642.2018.1428718
Todd, A. R., Thiem, K. C., & Neel, R. (2016). Does seeing faces of young black boys facilitate the identification of threatening stimuli?. Psychological Science, 27(3), 384-393. https://doi.org/10.1177/0956797615624492
Turner, R. N., & Brown, R. (2008). Improving children's attitudes toward refugees: An evaluation of a school‐based multicultural curriculum and an anti‐racist intervention 1. Journal of Applied Social Psychology, 38(5), 1295-1328. https://doi.org/10.1111/j.1559-1816.2008.00349.x
U.S. Department of Education, Office for Civil Rights. (2015). Protecting civil rights, advancing equity: Report to the president and secretary of education, under Section 203(b)(1) of the Department of Education Organization Act, FY 13–14. http://www2.ed.gov/about/reports/annual/ocr/report-to-president-and-secretary-of-education-2013-14.pdf
Vuletich, H. A., & Payne, B. K. (2019). Stability and change in implicit bias. Psychological Science, 30(6), 854-862. https://doi.org/10.1177/0956797619844270
Wallace, J. M., Goodkind, S., Wallace, C. M., & Bachman, J. G. (2008). Racial, ethnic, and gender differences in school discipline among U.S. high school students: 1991-2005. The Negro Educational Review, 59(1-2), 47–62.
Warikoo N., Sinclair S., Fei J., Jacoby-Senghor D. (2016) Examining racial bias in education: A new approach. Educational Researcher, 45(9), 508–514. https://doi.org/10.3102/0013189X16683408
Warring, D. F., Keim, J., & Rau, R. (1998). Multicultural training for students and its impact. Action in Teacher Education, 20(2), 56-63. https://doi.org/10.1080/01626620.1998.10462917
Wells, A. S., Fox, L., & Cordova-Cobo, D. (2016). How racially diverse schools and classrooms can benefit all students. Century Foundation. https://production-tcf.imgix.net/app/uploads/2016/02/09142501/HowRaciallyDiverse_AmyStuartWells-11.pdf
Whitford, D. K., & Emerson, A. M. (2019). Empathy intervention to reduce implicit bias in pre-service teachers. Psychological Reports, 122(2), 670-688. https://doi.org/10.1177/0033294118767435
State of the Science: Implicit Bias in Healthcare 2018-2020
State of the Science: Implicit Bias in Healthcare 2018-2020As a pervasive influence that affects social interactions across various domains, implicit bias has drawn substantial attention in healthcare research. Questions like why youth of certain racial and ethnic backgrounds more likely to be diagnosed with disruptive behaviors (Fadus et al., 2020), or why Black individuals assumed to have stronger pain tolerance than their White counterparts (Miller et al., 2020) are just a few of the questions addressed from implicit racial bias research. Whether positive or negative in valence, implicit racial bias for or against a group influences medical providers across all specialties and negatively impacts patient care (Cooper et al., 2012; Haider et al., 2011). Between 2013 and 2017 the Kirwan Institute for the Study of Race and Ethnicity published a series of reports of implicit bias literature that analyzed the scientific foundations and impacts of implicit racial bias within the healthcare system. These State of the Science reports chronicled numerous studies that documented alarming racial disparities that result from implicit biases held at both individual and institutional levels. Specifically, Kirwan’s analysis brought together empirical research illustrating the impact of implicit bias across multiple foci in healthcare, including clinical decision-making and medical education. The report series also underscored the need for further exploration of how implicit bias manifests itself and for interventions aimed at achieving equitable healthcare outcomes. This current report updates the state of science on implicit bias in the healthcare industry across three years: 2018, 2019, and 2020. Kirwan’s first implicit bias publication, State of the Science: Implicit Bias Review 2013, laid the groundwork for our subsequent reports by evaluating implicit bias in a range of professional sectors. Regarding healthcare, both the 2013 and 2014 State of the Science reports aggregated clear empirical evidence connecting implicit racial biases with racially disparate treatment decisions across various health conditions – ranging from acute coronary syndrome to HIV (Moskowitz et al., 2012; Stone & Moskowitz, 2011). Moreover, physician biases in both doctor-patient interactions and pain assessments were documented (Burgess et al., 2014; Chae et al., 2014; Sabin et al., 2009). The State of the Science reports from 2015, 2016, and 2017 added a new dimension of analysis: the role of medical schools. These three reports shared cumulative evidence from multiple studies (Gonzalez et al., 2014; White & Stubblefield-Tave, 2017; Zestcott et al., 2016), presenting a plethora of bias mitigation strategies focused on improving equitable decision-making by medical students and ultimately reducing healthcare disparities in clinical practice. These strategies, which addressed curriculum design at the institutional level and techniques like mindfulness meditation at the individual level, provided a framework for mitigating the effects of implicit bias during the early stages of a provider’s career.
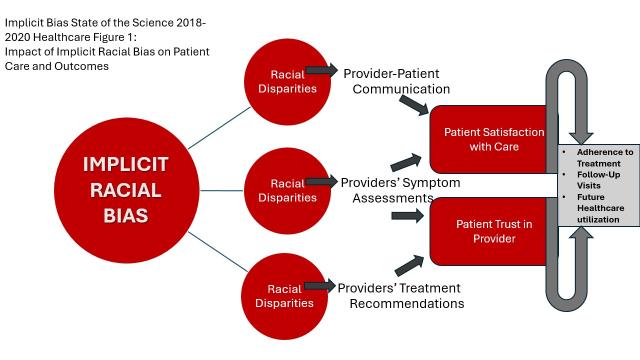
Since the publication of the landmark report, “Unequal Treatment” (Nelson, 2002), racial and ethnic treatment disparities are now one of the most widely examined topics in the field of healthcare. Three types of healthcare interactions have been consistently identified to contribute to differential treatments of patients based on race/ethnicity: provider-patient communication (see Burgess et al., 2019; Hagiwara et al., 2020; Lowe et al., 2020b), providers’ symptom assessments (see Fadus et al., 2020), and providers’ treatment recommendations (see Burgess et al., 2019; Hymel et al., 2018; Thomas, 2018). Figure 1 illustrates a series of patterns that have been observed across these dimensions. First, multiple reviews have documented that healthcare providers’ implicit biases negatively affect provider-patient communication dynamics, which in turn, can lead to lower levels of patient satisfaction with care and reduced trust in their provider (Miller et al., 2020). Patient satisfaction and trust in their provider are also well-established predictors of patients’ health-related behaviors such as adherence to treatment, follow-up visits, and future healthcare utilization (Stewart et al., 2013; Street et al., 2009). Second, suboptimal assessments of symptoms were also identified as a contributing factor to health disparities among racial and ethnic minority patients (Fadus et al., 2019; Hymel et al., 2018; Thomas, 2018). Last but not least, healthcare provider implicit bias is also associated with suboptimal treatment recommendations for racial and ethnic minority patients as compared to their White counterparts (Fadus et al., 2020; Hagiwara et al., 2020; Hymel et al., 2018; Thomas, 2018). In a similar vein, a non-trivial number of articles across the three-year period focused on the impact of implicit racial bias on patients under the age of 18, typically called pediatric patients (Fadus et al., 2020; Goodwin, 2018; Hymel et al., 2018; Johnson, 2020; Miller et al., 2020). Findings across this period revealed substantive similarities in the role of implicit racial bias between adult or pediatric cases, suggesting two important ramifications. First, such findings underscore the ongoing vulnerability of children of color in our healthcare system. Second, and perhaps even more troubling, negative childhood medical experiences may shape patients’ willingness to seek medical care later as adults (Pate et al., 1996), creating particularly challenging conditions for improving either healthy outcomes for patients themselves at the micro level or broader community health outcomes like rates of type II diabetes or infectious disease vaccination at the macro level.
In the current review, we follow the 2017 review by exploring and consolidating the research related to implicit racial bias in healthcare published between January of 2018 and December of 2020. For this industry-specific report we analyzed a total of 61 academic articles published between 2018-2020 in peer-reviewed journals. This number includes 18 published in 2018; 17 published in 2019, and 26 published in 2020. For more information about how we selected and analyzed articles, please go to our implicit bias introduction. Table 1 illustrates the variety of specialties covered across the time period. A clear variation exists with several specialties having more scholarship published in the arena than others; some specialties remain under- or unrepresented completely.
Table 1. Specialty Representation by Year 2018-2020*
*Specialties listed in alphabetical order; some articles fit multiple categories (e.g., pediatric psychiatry, surgical education)
**While COVID19 is not a formal category, we include it in anticipation of readers’ questions about the impact of the global pandemic on our analysis.
Specialty | 2018 | 2019 | 2020 | Total |
|---|---|---|---|---|
Dentistry |
| 1 |
| 1 |
Emergency Medicine |
|
|
| 1 |
Family Medicine |
| 1 |
| 1 |
Medical Education | 5 | 8 | 7 | 20 |
Mental Health (Psychiatry & Psychology) | 3 |
| 1 | 4 |
Miscellaneous General Articles | 4 | 2 | 4 | 10 |
Neurology |
|
| 2 | 2 |
Nursing | 1 | 2 | 1 | 4 |
Obstetrics | 3 |
| 2 | 5 |
Oncology |
|
| 2 | 2 |
Otolaryngology |
| 1 |
| 1 |
Pediatrics | 2 | 1 | 4 | 7 |
Radiology |
|
| 1 | 1 |
Surgery (all specialties) | 1 | 2 |
| 3 |
**COVID19 |
|
| 4 | 4 |
Especially relevant for this report, although both nurses and physicians work in challenging and high-stress environments that are conducive for implicit bias activation, researchers have raised concerns that current research on implicit bias in healthcare almost exclusively focuses on physician-patient interactions, which leaves a gap for further research on nurse- and/or medical staff-patient interactions (Crandlemire, 2020; Greene et al., 2018; Schultz & Baker, 2017). We therefore attend to the broader category of “healthcare provider” in this report to encompass practicing physicians, nurses, medical staff, interns and residents.
Understanding where the science has led scholars to date is an essential stimulus for further study. Our goal is to offer an accessible summary of implicit bias research in healthcare during this three-year window and to present insights for potential future research directions, including the development of effective interventions that contribute to the ultimate goal of establishing a more equitable healthcare system for all.
Implicit Bias in Healthcare: 2018
Implicit Bias in Healthcare: 2018Kirwan’s previous State of the Science reports emphasized differential treatment of patients due to implicit bias among healthcare providers (see also Burgess et al., 2014; Chae et al., 2014; Moskowitz et al., 2012; Sabin et al., 2009). Consistent with this theme, studies published in 2018 continued to investigate the pervasiveness of implicit racial bias within healthcare systems and its adverse impacts on the quality of care as well as patient outcomes. A total of 18 articles from the year 2018 were included in the article dataset. In the following section, we examine insights here as they pertain to the manifestation of implicit bias in healthcare. Specifically, we synthesize the findings regarding the potential negative impacts of implicit racial bias on patient care, including a discussion of disparate quality of care and differential standards of medical decision-making (Goodwin, 2018). The impact of implicit bias isn't confined to general healthcare alone but extends its reach to various specialized healthcare services, each presenting unique challenges.
Our 2018 Healthcare State of the Science takes a deep dive into the question of who in the healthcare system is influenced by implicit bias. We found articles focused on healthcare providers across specialties (Maina et al., 2018; Tajeu et al., 2018); medical trainees (Backhus et al., 2019; Hernandez, 2018); and mitigation strategies. The three articles that explicitly focus on mitigation are combined with recommendations from other years into a single cumulative mitigation strategies section for the healthcare sector. Articles published in 2018 affirm the pervasiveness of implicit racial bias among providers from multiple specialties (pediatrics, obstetrics, mental health) and trainees undergoing medical education (medical students and residents). Even patients themselves (Greene et al., 2018) are susceptible to being influenced by implicit racial bias as they make decisions about their healthcare.
Impact of Healthcare Provider’s Implicit Racial Bias on Patient Care
Our data collection strategy uncovered three medical specialties that used a variety of methods (quantitative, qualitative, mixed methods and meta-analysis) to arrive at their conclusions. In this section we focus on obstetrics, pediatrics, and mental health implicit racial bias research published in 2018. We cover additional specialties in 2019 and 2020 as applicable based on the results of our data collection strategy. All three of the specialties we analyzed for 2018 acknowledged the intersection of the healthcare system with other important and relevant systems that are also grappling with significant racial disparities: the child welfare system (obstetrics and pediatrics) and the criminal justice system (mental health).
Obstetrics
Obstetrics and gynecology as a medical specialty has a particularly fraught history with explicit racial bias and discrimination, which has had a direct effect on the quality of patient care. Several articles published in 2018 allude to this broader history as well as provide evidence of ongoing implicit racial bias. Brenda Pereda and Margaret Montoya (2018) provide a broad review of the role of implicit bias and note specifically the history of non-consensual medical experimentation on enslaved women and forced sterilization of Latinas as part of the embedding of bias. In a similar vein Erin Thomas (2018)’s study of bias among lactation consultants suggests that such bias originates from larger inequalities in society and must be addressed at their root.
Through semi-structured interviews with 36 lactation consultants, Thomas (2018) documented instances of race-based discrimination against patients seeking lactation care and connected these findings to the implicit bias literature. Through an analysis of interview transcripts, the researcher identified three subthemes of implicit bias, including lower quality and less quantity of care. Thomas used actual statements given by the interviewees to show how Black and Hispanic mothers were denied proper assistance with breastfeeding because healthcare providers believed it would be a waste of resources. Similar biases toward various Asian groups were also observed, particularly those who spoke English as a second language. Thomas (2018) explicitly connected these biases to quality of care, finding that White patients received more services and less referrals to social services in lactation care compared to Black patients. This was especially prevalent in cases where a patient used drugs or showed signs of mental illness. Although the study did not directly measure implicit bias, it presented us with compelling evidence of its existence. Of special interest to our analysis, Thomas noted negative pediatric impacts of positive implicit racial bias, where White infants were at higher risk when parents displayed evidence of drug abuse or mental illness left unacknowledged by lactation consultants.
This study was accompanied in 2018 by the publication of a national study of 286 perinatal physicians by Natasha Shapiro and colleagues (2018), which used a vignette strategy to explore the role of implicit bias regarding both race and socioeconomic status. In this study, physician participants were instructed to view a vignette featuring a female patient in imminent labor. The patient's race was indicated by a photograph of either a White or Black individual, while their socioeconomic status was implied by mentioning the care is provided by either a "Private Obstetrician" for high socioeconomic status or by the "Resident OB clinic" for low socioeconomic status. After being randomly assigned to view one of the four versions of the vignette, participants were then asked about how likely they would recommend the patient for intensive care versus comfort care.
Following this choice, participants’ implicit biases were also measured through two Implicit Association Tests (IATs) focused on race and socioeconomic status respectively. The results revealed that the participating physicians demonstrated an implicit preference for White patients and those with higher socioeconomic status. However, it was found that these implicit biases did not influence the physicians' treatment decisions based on the patient's race. The researchers suggested that this could be a result of physician’s higher self-awareness of racial biases and their impact on decision-making, making them more cognizant of not letting these biases influence their recommendations. The researchers also started with a sample of 971 physicians who initially started the study; 685 physicians did not complete the entire study so there is more work to be done to understand the relationship between implicit racial bias and implicit socioeconomic bias in obstetrics. Interestingly, some prior research suggests that someone whose behavior does not necessarily reflect the biases might still be influenced by social or cultural norms in their responses to IATs Fazio & Olson (2003), which is consistent with some of the literature in medical education that points to mitigation strategies that focus on the meso- and macro-level of analysis. We take up this point in the mitigation strategies section of this report.
Pediatrics
As with obstetrics scholarship in 2018, pediatrics research published in the same year also focused on the impact of implicit biases on quality of care in both qualitative and quantitative studies. Michele Goodwin (2018)’s analysis of the Jahi McMath case, where she documented the tragic experiences of a 13-year-old girl who suffered severe complications after receiving a routine tonsillectomy, which is the second most commonly performed pediatric surgical procedure in the United States (Jaryszak et al., 2011). Goodwin cited several statements from Jahi’s family questioning whether she received the standard quality of care. While acknowledging the tragedy of McMath’s death Goodwin suggested that there are numerous social implications regarding the influence of healthcare providers’ implicit biases upon the quality of care received by patients who are members of minoritized racial groups.
In a similar vein Kent Hymel et al. (2018) conducted a cross-sectional analysis of 500 pediatric patients under three years of age with acute head injuries to examine the potential influence of implicit bias among physicians who specialize in Abusive Head Trauma (AHT). Here the researchers used the evaluation and reporting frequencies of AHT as an indirect measure of implicit racial bias. Their findings showed that racial and ethnic minority patients were evaluated and reported more frequently for suspected AHT than White (non-Hispanic) patients, which is considered an indicator of implicit racial bias in reporting standards. Similar to the Thomas (2018) study, Hymel et al. (2018) suggest “positive” implicit racial bias, like giving White parents the “benefit of the doubt,” when assessing for potential child abuse, can have negative outcomes for White non-Hispanic babies under three years old. The consequences are critical, even if they exist predominantly in lower-risk patients, because delays in AHT diagnosis have been shown to lead to re-injury or even death.
Both obstetrics and pediatrics authors suggest that having too many false positives among minoritized caregivers in AHT cases and too few positives in lactation cases are detrimental both for the young patients themselves (infants and children up to three years old) but also for the parents, who either face unwarranted referrals to child welfare services or law enforcement OR do not get adequate treatment for the drug dependence or mental health concern, leaving children at risk in either outcome.
Mental Health
Four (4) studies published in 2018 analyzed the role of implicit racial biases in mental healthcare, using a variety of empirical methods. Similar to their peers in other specialties, healthcare providers in the mental health field also may hold similar levels of implicit bias against certain patients based on their race, ethnicity, and sexual orientation (Hall et al., 2015; Merino et al., 2018; Snowden, 2003). That said, Yesinia Merino and colleagues (2018) conclude that mental health care is particularly vulnerable to the effects of an individual provider’s implicit racial bias because it heavily relies on one-on-one services where a single provider acts as the gatekeeper to care. Ivy Maina and colleagues (2018) conducted a meta-analysis to consolidate findings of 37 studies published between 1997 and 2015. Their review found that there is growing evidence suggesting that similar to the general U.S. population, a substantial number of healthcare providers across different training levels and disciplines hold implicit biases against Black, Hispanic, American Indian, and dark-skinned individuals more broadly. Maina and colleagues found that studies focused on real-world patient care yielded more consistent findings, which revealed an association between higher implicit bias and less favorable patient-provider interactions.
Merino and colleagues (2018) argued that the potential impact of negative implicit bias reaches various aspects of mental health care, encompassing not only clinical screening but also diagnosis, treatment processes, and crisis response. Furthermore, they also explored the intersection of implicit bias in mental health care and criminal justice institutions. The authors emphasized the importance of this exploration as prison systems have become one of the largest mental health providers in the U.S. (James & Glaze, 2006). In their conclusion, Merino and colleagues reiterated the need to understand how individual practitioners' implicit attitudes influence the delivery of mental health services and treatment effectiveness. Additionally, the authors also urged future investigations to not overlook how structural inequities within the mental health system could perpetuate implicit bias. The structural inequities they identified include the lack of diversity in the mental health workforce and among mental health educators, evidence-based practices that are centered on a majority-group framework, and the lack of diversity on the boards of mental health agencies (Merino et al., 2018).
While Javeed Sukhera et al. (2018b) and George Bermudez (2018) focus more on mitigation strategies, each documents the presence of implicit racial bias among mental health care providers prior to engaging in mitigation. Sukhera et al. focuses on a group of psychiatry faculty and residents, while Bermudez focuses on a group of faculty, students and administrators from various disciplines using psychoanalytic techniques of social dreaming. Analyses of their proposed mitigation strategies in connection with other research can be found in the cumulative mitigation strategies section.
Conclusion
The studies discussed in the 2018 State of the Science use a variety of methods to document the ongoing challenges presented by the role of implicit racial bias among healthcare providers and implicit racial bias’s connection to systemic barriers in the social welfare and criminal justice systems. While recommendations for mitigation are explored in a different section of this report, the articles described here offer both general and specialty-specific ideas for future research. Both Maina et al. (2018) and Thomas (2018) identified a need to move beyond a focus on physicians’ implicit bias to include other types of healthcare providers in the mental healthcare specialty, with Thomas (2018) noting the particular role that lactation consultants play with new parents of infants. To meet this need Tajeu et al. (2018) conducted a statewide study of 107 healthcare staff, which included physicians, nurses, and non-MD/RN personnel such as receptionists. The authors found that White staff members had higher implicit racial bias against Black patients than the physicians or nurses, identifying a potential gap for both further research and mitigation strategy development.
As we noted in the general introduction to the Healthcare State of the Science report, the “who” in healthcare has continued to expand beyond simply physicians. Similar to healthcare providers and non-MD/RN staff, patients can also exhibit implicit racial bias, especially when selecting their physicians, but this also remains a relatively understudied area. Jessica Greene and colleagues (2018) asked study participants to hypothetically choose from four physicians based on their performance quality information. Among the four, two physicians had top performance ratings and two had lower quality performance ratings. The study manipulated the names of the top-performing physicians to represent different races/ethnicities and genders. The findings revealed that respondents more frequently selected a physician with a typically White male name compared to the same physician with either an African American male, African American female, or Middle Eastern name. This bias was more pronounced among White respondents. Greene and colleagues cautioned that it remains unclear if this bias found in an isolated experiment setting can translate into real-world physician selection. If it does, however, it could result in racial and ethnic minority and women physicians having smaller patient panels (Ly et al., 2016). Given the increasing enrollment in health plans with limited provider networks (Polsky & Weiner, 2015) and the painfully slow but steady diversification of the medical profession, the potential influence of implicit bias in patients' choice of new physicians becomes particularly relevant.
Implicit Bias in Health/Health Care: 2019
Implicit Bias in Health/Health Care: 2019Our review of implicit racial bias research published in 2019 includes 17 articles. Whereas research in 2018 provided multiple pieces of scholarship that offered a sense of depth in particular specialties (obstetrics, pediatrics, mental health), 2019 research featured breadth across eight (8) specialties and depth in medical education (4 articles) and mitigation strategies
(10 articles). The medical education articles complement two articles published in 2018 (Abelson et al., 2018; Hernandez, 2018), which did not on their own constitute a set of findings. We therefore further dissect how implicit racial bias plays a role in patient care by exploring it in medication education in the first section and then across specialties in the following section. Mitigation articles are discussed in the cumulative mitigation strategies section of this report.
Impact of Healthcare Providers’ Implicit Racial Bias
Medical Education
No matter the industry – healthcare, education, or criminal justice – implicit racial and ethnic bias has been found to play a heightened role in cognitive functions whenever there are high stress / high cognitive load or ambiguous environments, to the point of being settled science. While many healthcare providers chide television and film representations of healthcare, there is one thing they do not contest: working as a healthcare provider is stressful and so is the training. In other words, medical trainees (e.g., medical or nursing students, interns, residents) are experiencing high cognitive loads in learning contexts which are uncertain (Johnson et al., 2016) and high stakes (medical care). So it is not surprising to learn that medical students and residents are more likely to have their preexisting implicit biases translated into explicit patient-care-related outcomes. Two longitudinal quantitative studies – one of 3,756 medical students across 49 different medical schools (Burgess et al. 2019) and one of 3,392 medical residents across various specialties – document this phenomenon. Liselotte Dyrbye and colleagues (2019) conducted a study to investigate medical residents’ implicit bias and their symptoms of burnout. A total of 3,392 non-Black participants across various specialties completed three point-in-time questionnaires: during their fourth year of medical school, as well as at the second and third years of residency. The findings showed that 45.2% and 41.3% of the sample experienced symptoms of burnout and depression, respectively. Moreover, after controlling for confounding variables such as demographics and specialty, burnout symptoms in the second year of residency were found to be positively associated with implicit racial biases a year later. Considering the widespread occurrence of burnout symptoms among medical residents and the adverse link between implicit racial bias and suboptimal care, Dyrbye et al. argued that signs of burnout could contribute to inequalities in healthcare delivery. Both medical residents and medical students form part of the essential pipeline for future healthcare providers.
Medical education research published in 2019 took two directions; exploring trainees’ existing implicit racial biases and the potential impact of such implicit biases on patient care and diversity of the pipeline, which is a critical pathway for improving the provision of culturally competent care. Both medical residents and medical students form part of the essential pipeline for future healthcare providers. Two articles looked at implicit racial bias among medical students, concluding that medical students’ implicit racial bias can have an impact on patient care.
Diana Burgess et al. (2019) collected data on political ideology and implicit bias from a sample of medical students. Using a stratified random sampling strategy, they recruited a total of 3,756 students in their first and fourth years of study from 49 medical schools. The researchers found that first-year students’ political ideology was associated with their implicit bias in year four. Specifically, a greater conservative political orientation in year one was linked to higher implicit racial bias against Black individuals in their final year of medical school. Over the duration of the study, a stronger initial conservative political ideology also predicted increased explicit attitudes toward stigmatized groups, reduced internal motivation to regulate racial prejudice, diminished levels of empathy toward patients, and decreased levels of patient-centered attitudes at a later time point. These correlations remained consistent across different medical schools and were not influenced by students' race or geographic location. Burgess and colleagues also noted that conservative ideology may align with characteristics like conscientiousness, self-control, and a sense of duty, which could potentially be utilized to improve care for marginalized populations. They did not, however, test any mitigation strategies, suggesting instead that further investigation is necessary. Second, Christine Motzkus and colleagues (2019) examined two cohorts of pre-clinical medical students enrolled in a determinants of health course, analyzing 250 deidentified essays from the course itself. More about Motzkus et al.’s findings can be found in the mitigation strategies section.
The second thread of medical education research in 2019 focused on the pipeline into medical school. Building on Abelson et al.’s 2018 study of the lack of diversity in the surgical specialty, Leah Backhus and colleagues (2019) assess problems presented by implicit racial bias and implicit gender bias. Backhus et al. found that the representation of African American surgeons at all levels of the academic hierarchy, including tenure, either remained stagnant or declined between 2003 and 2006. Additionally, retention rates were significantly higher for White assistant professors, whereas Black assistant professors had the lowest promotion rates across all specialties. Backhus et al.’s 2019 study recognized the pervasive nature of implicit racial bias throughout the recruitment and training processes for future physicians. The authors pointed out that racial and ethnic minorities in both medicine and medical education are significantly underrepresented. According to the data collected between 2014 and 2015, Black individuals comprised only 5.7% of medical students and 6.2% of general surgery residents. These figures starkly contrast with the 12.4% representation of Black individuals in the U.S. population. Similarly, despite Hispanics constituting 17.4% of the U.S. population, only 4.5% of medical students and 8.5% of general surgery residents represent this demographic (Abelson et al., 2018). Backhus and colleagues (2019) suggested such racial disparities in medical education could be partially due to implicit racial biases held by influential individuals in the system. The authors referenced a study that examined the implicit biases of 140 members of medical school admissions committees at a Midwestern university. Using the Black-White IAT, the study found that all groups of the committee exhibited levels of implicit preference for White males and faculty were shown to have the highest implicit bias scores (Capers et al., 2017). Moreover, underrepresentation of minorities in medical education at the faculty level could directly influence the recruitment, mentoring, and retention of minority students (Rodriguez et al., 2014).
Healthcare Providers
Four (4) studies, each in a different specialty (trauma care, otolaryngology, nursing, and dentistry), continued to use a broad definition of healthcare provider beyond the narrow focus on MDs (Narayan, 2019; Tajeu et al., 2018; Zebib et al., 2019). While some 2019 medical education studies emphasized the stress and ambiguity aspects of the healthcare context, another study emphasized the population context to evaluate whether racial and socioeconomic diversity would mitigate the existence of implicit racial bias in trauma care. Laura Zebib and colleagues (2019) recruited 91 participants from ten (10) healthcare professions in Miami, Florida. Their study found that trauma healthcare professionals in a multicultural city exhibited reduced levels of implicit racial and socioeconomic bias compared to the average implicit bias amount White surgeons in the U.S.
In a summary of the associations among implicit bias and patient safety as well as the quality of care, Karthik Balakrishnan & Ellis Arjmand (2019) underscored that professional healthcare providers are as susceptible as the general population to implicit social and cultural biases (Zestcott et al., 2016). Drawing on studies conducted by Plaisime et al. (2017) and Penner et al., (2016), Balakrishnan and Arjmand suggested that the implicit biases not only influence assessment made by clinicians and providers’ decision-making processes in treatment, but also affect how patients perceive their encounters with healthcare professionals, which impacts patient satisfaction and their confidence in the care received.
Mary Narayan (2019) also discussed the presence of implicit bias, suggesting that such bias influences the relationships between providers and patients, the quality of care delivered, and the psychosocial well-being of patients. Regarding the provider-patient relationship, biases may lead to perceiving Black patients as having inferior communication skills and being less warm, friendly, and team-oriented. This perception can result in decreased patient adherence, fewer return visits, and diminished trust in healthcare providers (Chapman et al., 2013). Furthermore, implicit biases may manifest as spending less time listening to Black patients and assuming that Black and Hispanic patients are less likely to adhere to treatment and cooperate compared to White patients (Zestcott et al., 2016). In terms of the quality of care, studies have shown that implicit bias influences diagnoses, treatment recommendations, the thoroughness of patient histories, and the frequency of tests ordered (FitzGerald & Hurst, 2017). Lastly, implicit biases can also affect patients' health outcomes, impacting factors such as social integration, levels of depression, and overall life satisfaction (Hall et al., 2015).
Neha Patel et al. (2019) implemented a cross-sectional survey at the University of Cagliari, Italy. Fifty-seven qualified dentists working in the endodontic department of one hospital participated in the survey. These examiner respondents were randomly assigned to review a clinical vignette featuring either a Black or White patient presenting a decayed tooth and related symptoms of irreversible pulpitis, which signals that the innermost layer of a tooth is no longer able to heal itself. Both canal treatment and extraction were viable treatment options. However, the loss of a tooth can result in compromised aesthetics, lower biting stability, and replacement options (such as fixed partial dentures or implants) may result in damage of adjacent teeth (Al-Quran et al., 2011; Saunders & Saunders, 1998). The examiner participants were tasked with assessing the likelihood that the patient’s symptoms were due to irreversible pulpits, providing their treatment recommendation, and indicating the strength of this recommendation.
Implicit racial bias held by respondents was measured using the Brief Implicit Association Test (BIAT) (Nosek et al., 2014). Across both conditions, 91.23% of the examiners participating in the study exhibited a pro-White implicit bias. Additionally, they were significantly more inclined to recommend root canal treatment for White patients and extraction for Black patients. Patel and colleagues suggested that the preference to recommend tooth extraction to Black patients might stem from assumptions about their socioeconomic status, which leads the examiners to believe that Black patients may not be able to afford root canal treatment. While this might be perceived as an empathetic gesture to avoid causing financial strain, the authors highlighted that it still reflects bias.
Conclusion
In sum these 2019 articles continue to articulate the harms that can ensue with failure to address implicit racial bias in healthcare. They complement those published in 2018 in terms of a focus on expanding scholars’ and clinical practitioners’ attention to broadening the types of healthcare providers studied, providing empirical and meta-analytical evidence of an existing problem that requires mitigation.
Implicit Bias in Health Care: 2020
Implicit Bias in Health Care: 2020The year 2020 was momentous in healthcare due to the sudden and acute onset of the COVID19 global pandemic. Our data collection strategy resulted in a total of 25 studies that were published in 2020 about implicit racial bias. Similar to our findings in 2019, the largest number of articles (11) were focused on mitigation strategies, followed by COVID19, and pediatrics. Aside from pediatrics, specialties were again represented broadly instead of deeply, with articles at either the broad cross-sectional level (Bonica et al., 2020; Chuang et al., 2020; Hagiwara et al., 2020) or as a single study in emergency medicine (Manchanda & Macias-Konstantopoulos, 2020), Neurology (Charleston et al., 2020), Obstetrics and Oncology (Lowe et al., 2020a; Lowe et al., 2020b), or Radiology (Maxfield et al., 2020). As was the case with articles published in 2018 and 2019, the findings from these studies will empower us to chart a clearer map for understanding how implicit bias may have detrimental effects on patient care, including specific dimensions like provider-patient communications, treatment recommendations, and health outcomes more broadly.
Impact of Healthcare Providers’ Implicit Racial Bias on Patient Care
Pediatrics
Although there is growing evidence of implicit bias favoring White patients over Black and Hispanic patients in general (Maina et al., 2018), most studies have used Implicit
Association Tests with adult-based race vignettes. One evolution in implicit racial bias research in 2020 was the improved utilization of age-specific IAT measures. Results from all three 2020 pediatric studies in our dataset affirm that implicit racial bias affects medical trainees (medical students and residents) as well as established physicians with little to no impact of patient age on the level of healthcare provider bias. Together these findings together draw attention to the presence of biased racial attitudes among healthcare providers toward both adult and pediatric patients, underscoring the vulnerability of children within the healthcare system.
In a review of implicit bias in pediatric physicians, Tiffani Johnson (2020) drew on two studies that compared measures by using both adult and child race vignettes to test heath care providers’ implicit bias and highlighted that children are also vulnerable to biased attitudes held by their health care providers (see also Thomas, 2018; Hymel et al., 2018). The two studies reviewed by Johnson were both conducted in the emergency department setting and examined implicit racial bias among physicians towards children. In one study, a majority of resident physicians from a pediatric emergency department showed pro-white/anti-black racial bias on both the Adult Race IAT (85%) and Child Race IAT (91%). Notably, there were no significant differences in the levels of implicit bias toward adults versus children. Prior research also affirms that levels of implicit bias did not vary based on resident demographic characteristics like gender or medical specialty when comparing pediatric resident physicians with emergency medicine residents (Johnson et al., 2016). In another study involving emergency department providers at five hospitals in the Midwest, a significant majority (84%) exhibited implicit bias favoring White children over American Indian children.
Racial and ethnic disparities in the diagnosis of disruptive behaviors have similarly received ongoing scholarly attention (Cameron & Guterman, 2007; Feisthamel & Schwartz, 2009; Mizock & Harkins, 2011). Previous studies have identified a tendency for Black and Latino youth from urban and low-income backgrounds to be overrepresented in this type of diagnosis (Cameron & Guterman, 2007). On the contrary, these same groups of minority youth are less likely than their non-Hispanic White counterparts to receive a diagnosis of ADHD (Coker et al., 2016). Facing the same group of young vulnerable patients, Matthew Fadus and colleagues (2020) presented a review that focused on disparities in the diagnosis of psychiatric disorders, specifically pertaining to oppositional defiant disorder (ODD), conduct disorder (CD), and attention-deficit/hyperactivity disorder (ADHD). Fadus et al. (2020) linked this concerning pattern to implicit biases held by clinicians, which may lead them to over-pathologize behaviors of ethnic and minorities as more disobedient and dangerous (see also Clark, 2007).
Third and finally pain-related disparities have been a longstanding concern in healthcare studies (e.g., Anderson et al., 2009; Campbell & Edwards, 2012; Green et al., 2003; Tait & Chibnall, 2014). Previous research found that providers are influenced by implicit racial bias, perceiving African Americans as having a higher pain tolerance than other racial and ethnic groups (Anderson et al., 2009). Megan Miller and colleagues (2020) assessed providers’ implicit bias in pain-related decision making in a pediatric medical setting. Their study sampled 129 medical students, and the results were consistent with the findings of previous studies, showing that the medical students assumed that African Americans had stronger pain tolerance than their White counterparts. It was also found that providers were more likely to recommend opioids for African American pediatric patients than White patients, which could lead to potentially harmful over-prescription for Black pediatric patients. These findings extended the scope of pain tolerance bias research that previously focused on acute pains, showing that providers held the same type of implicit racial bias applies when it pertains to chronic pain tolerance. These findings underscore the alarming reality that implicit racial biases in pain perception cross age ranges to include children under the age of 18.
COVID19
The COVID-19 pandemic disrupted and transformed the field of healthcare in ways that few could have imagined. As the pandemic spread across the world in 2020, it became increasingly evident that different racial and/or ethnic groups had varying COVID-related incidence and mortality rates (Wadhera et al., 2020). Our dataset included five (5) early studies that explored the impact of implicit racial bias on COVID-19 as a public health issue. Moreover, a sudden increase of stigmatizing media reports about the virus’ origins also fueled implicit and explicit biases against Asian Americans (Darling-Hammond et al., 2020). The racial implications of the murder of George Floyd (Davis-Martin, 2020) and media linkages of COVID-19 to people of Asian descent alike posed significant challenges in health care outcomes. As we illustrated in the general introduction to the State of the Science, patient-provider trust plays a direct role in health outcomes. Moreover, studies by both Burgess et al. (2019) and Bonica et al. (2020) suggest provider ideology is increasingly playing a role in both provider location (Bonica et al.) and patient care (Burgess et al.).
Using data from Project Implicit, a non-profit platform that provides IATs as a “virtual laboratory” for studying implicit social cognition on the Internet, Thomas and colleagues (2020) analyzed anti-Black bias among non-Hispanic Whites across 2,994 counties. It was estimated that high levels of implicit bias at the county-level was positively associated with high COVID-19 incidence rate among Black Americans. This study was the first to test and report the associations between county-level implicit racial bias and COVID-19 incidence and mortality rates in the United States (Thomas et al., 2020). The authors noted that further research is needed to better understand the relationship between implicit racial bias and disparities caused by an infectious rather than chronic disease.
The COVID-19 pandemic not only shed light on the detrimental effects of healthcare providers' implicit racial bias but also sparked discussions about the potential influence of implicit bias as perceived by patients in physicians. Davis-Martin (2020) chronicled their experiences as a behavioral health provider to help their patients deal with anxiety about upcoming procedures. The patient in this case experienced heightened anxiety due to the combined impact of COVID-19 and racial tensions prevalent at the time. In his expression of concern to the author, the patient talked about how he feared that the riots featured in the news might negatively affect perceptions of his racial group. Consequently, the patient felt uncomfortable disclosing this fear to his White primary care provider, worrying the quality of care he receives may be negatively impacted, stating, “What if my surgeon does a bad job because they think I hate the police or America?” This narrative offered a unique perspective from a Black patient’s point of view, showing that even the mere suspicion that one’s physician may have implicit bias is enough to alter a patient’s decision-making process, leading to hesitation in scheduling a surgery appointment with a White healthcare provider.
While African American communities were disproportionately burdened by higher COVID-19 incidence and mortality rates, the pandemic also sounded an alarm about the effects of stigmatizing media on the health and welfare of Asian Americans. On March 8, 2020, a 650% increase in Twitter retweets using the term “Chinese virus” and affiliated terms was observed.
The use of these terms had an 800% increase in conservative news media articles the following day. Darling-Hammond and colleagues (2020) analyzed data from non-Asian participants of the Project Implicit “Asian Implicit Association Test” from 2007-2020. The results showed that Implicit Americanness bias (i.e., the subconscious belief that individuals of European origins are more “American” than those of Asian origins) declined from 2007 through early 2020. The trend was reversed, however, following the explosion of use of racially stigmatizing language on media outlets. This trend reversal is consistent with the longstanding stereotype of Asian
Americans as “perpetual foreigners;" the researchers argued that it may also lead to increases in discriminatory behaviors, with adverse mental and physical outcomes for those who experience discrimination. While these articles were published early in the pandemic cycle, numerous articles have sadly documented tremendous increases in violence and discrimination against Asian Americans well beyond the healthcare sphere in the shadow of the pandemic (Chan et al., 2024).
Implicit Racial Bias Across Specialties
In 2020, new studies on differential treatment in healthcare focused more on specific types of providers and specialties. A systematic review showed that health care providers from various backgrounds and levels of training hold implicit biases against non-White individuals (Maina et al., 2018). Similar results were also found in emergency medicine and radiology in more up-to-date studies published in 2020. Examining 40 emergency medicine faculty, Cleveland Manchanda and Macias-Konstantopoulos (2020) found that 45% of their sample reported IAT results with an implicit preference for Whites. Moreover, Maxfield and colleagues (2020) examined the IAT results reported by 31 faculty participants at three academic radiology departments. The results of this study revealed that 71% of participants exhibited implicit anti-Black bias. Adding to these studies that primarily focused on physician implicit bias, Lynn Crandlemire (2020) underscored in her review of implicit bias’s impact on caring, that the majority of nurses are susceptible to implicit racial bias as well (see also Haider et al., 2015).
Previous research has also shown that implicit racial bias held by clinicians can negatively impact communication with patients, which can foster decreases in patient trust, engagement, and adherence to treatment (Zestcott et al., 2016). Chenery Lowe and colleagues (2020a, 2020b) extended this line of research to the field of genetic counseling to examine counselors’ implicit bias with mixed findings. Using Linguistic Inquiry Word Count (LIWC) and Roster Interaction Analysis System (RIAS), they examined the influence of implicit racial bias in genetic counselors’ facilitation of emotional and cognitive processing (Lowe et al, 2020a). Contradictory to the conventional findings in studies with clinicians, they did not find an association between genetic counselors’ pro-White implicit bias and their communicative behavior during sessions. The researchers suggested that it is possible that the LIWC measure was not sensitive enough to capture an implicit bias effect in counseling sessions, or the small sample size used in the study could have limited their ability to detect associations between cognitive and emotional processing and IAT scores.
Adopting a different approach to focus on counselors’ framing of information, the researchers conducted another study to investigate whether genetic counselors’ implicit racial bias affected their communication style with simulated minority clients (Lowe et al., 2020b). The study involved a sample of sixty genetic counselors, primarily consisting of females (92%) and individuals identifying as non-Hispanic/Latino White (90%). Participants completed the Race IAT assessment and engaged in simulated counseling sessions with clients (17 sessions with simulated White clients and 43 sessions with simulated African American or Hispanic Latino clients). The information framing employed by counselors in the recorded sessions was analyzed using a genetic counseling-specific adaptation of RIAS coding. The results showed that implicit racial bias may negatively impact clinicians’ communication style. Genetic counselors with higher pro-White implicit bias provided less informational individuation and made fewer facilitation and activation statements to minority clients compared to their White counterparts. It was also found that with counselors who scored higher on the IAT, minority clients asked fewer medical questions and disclosed less information (Lowe et al., 2020b). These results highlighted that the implicit racial bias held by a genetic counselor likely affects counselor-patient communication in both directions.
Conclusion
While much has been written about COVID19 and explicit bias, discrimination, and even violence, particularly against African Americans in light of George Floyd’s murder and against Asian Americans in light of the pandemic, we kept a strict focus on implicit racial bias for this 2020 analysis. For example, Thomas’ 2020 results noted that implicit bias was significant under a single circumstance, while explicit bias was consistently statistically significant. As we’ve already noted, the negative effects of implicit racial bias are real, and that is why we have kept our attention focused on them. We take up lingering questions about research impact along with those from Maina et al., 2018 and other articles in the Conclusion and Directions for Future Research section of this report.
Mitigating Implicit Racial Bias in Health/Healthcare
Mitigating Implicit Racial Bias in Health/HealthcareAs discussed in the previous sections, the influence of implicit bias is evident in both medical education and everyday healthcare practices, thereby subtly shaping the learning experiences of students and the development trajectories of healthcare professionals. Without recognition of and adequate intervention for implicit bias, individuals immersed in these systems may inadvertently promote inequitable practices. In this section, we present a compilation of articles published between 2018 and 2020 that explored strategies aimed at mitigating implicit bias within the healthcare field. A total of 30 articles were analyzed for this section; this constitutes almost half of our 61-article dataset. Table 2 lists the specialties and citations for readers seeking further specialty-specific details.
Table 2. Implicit Bias Mitigation Strategy Research 2018-2020 by Specialty
Specialty | Total Number of Articles Analyzed in this Section | Citations |
|---|---|---|
Family Medicine | 1 | Sherman et al., 2019 |
Medical Education | 20 | Avant & Gillespie 2019; Backhus et al., 2019; Burgess et al., 2019; Capers et al., 2020; Caruso-Brown et al., 2019; Gatewood et al., 2019; Gonzalez et al., 2019; Hernandez 2018; McClinton & Laurencin, 2020; Motzkus et al., 2019; Muntinga et al., 2020; Onyeador et al., 2020; Perdomo et al., 2019; Sherman et al., 2019; Stone et al., 2020; Sukhera et al., 2018a; Thomas & Booth-McCoy 2020; Tsai & Michaelson, 2020 |
Mental Health | 2 | Bermudez, 2018; Fadus et al., 2019 |
Neurology | 1 | Charleston & Spears, 2020 |
Nursing | 4 | Alspach 2018; Crandlemire, 2020; Gatewood et al., 2019; Narayan, 2019 |
Obstetrics / Gynecology | 1 | Pereda & Montoya, 2018 |
Oncology | 1 | Graboyes et al., 2020 |
Otolaryngology | 1 | Balakrishnan & Arjmand 2019 |
Palliative Care | 1 | Chuang et al., 2020 |
Pediatrics | 1 | Fadus et al., 2019 |
Pharmacy | 1 | Avant & Gillespie 2019 |
Surgery | 1 | Backhus et al., 2019 |
These interventions cover various career stages, from medical student education and residency program matching to professional development for healthcare providers and medical school faculty retention. Ranging from widely practiced awareness training to examinations of the medical school environment, these strategies address individual, institutional, and systemic factors. Consistent with our other 2018-2020 State of the Science Reports, we define individual-level factors as those factors that influence individuals’ likelihood to cognitively but unconsciously rely on implicit racial bias – including but not limited to previously established influences as cognitive load (fatigue, stress, burnout) and ambiguous decision / decision complexity. While these factors are influenced by the situation, individuals experience them individually. We define institutional factors as factors that shape the context at the meso-level, like at the level of the entire medical or nursing school, or across an entire specialty nationally. Finally, we define systemic factors as the set of factors that transcend or intersect with healthcare. For example, cultural and historical stereotypes are not usually unique to the healthcare system. Similarly, while the child welfare or criminal justice system intersects with the U.S. healthcare system, they are not synonymous with the healthcare system. We organize this section accordingly. Table 3 presents a summary of the mitigation strategies derived from our review of healthcare-specific strategies discussed among the articles we analyzed. Each strategy is hyperlinked to facilitate easier navigation for readers.
Table 3. Mitigation Strategies Discussed in Healthcare Implicit Racial Bias Research, 2018-2020
| Strategy | Citations |
|---|---|
| Individual Strategy 1: Awareness Intervention | Alspach, 2018; Avant & Gillespie, 2018; Backhus et al., 2019; Balakrishnan & Arjmand, 2019; Motzkus et al., 2019; Sherman et al., 2019; Sukhera et al., 2018a; White et al., 2018 |
| Individual Strategy 2: Adopt Evidence-Based Mitigation Techniques | Backhus et al., 2019; Balakrishnan & Arjmand, 2019; Bermudez 2018; Narayan, 2019 |
| Individual Strategy 3: Design Interventions with Resistance in Mind | Alspach, 2018; Backhus et al., 2019; Gatewood, 2019; Gonzalez et al., 2019; Sukhera et al., 2018b |
| Institutional Strategy 1: Incorporate Advances in Curriculum Development | Bermudez, 2018; Burgess et al., 2019; Fadus et al., 2019; Hernandez, 2018; Motzkus et al., 2019; Stone et al., 2020; Tsai & Michaelson, 2020 |
| Institutional Strategy 2: Pilot Novel Curricula | McClinton & Laurencin 2020; Perdomo et al., 2019; Thomas & Booth-McCoy, 2020 |
| Institutional Strategy 3: Adopt a Nuanced Approach to Structural Racism | Backhus et al., 2019; Capers et al., 2020; Chuang et al., 2020; Fadus et al., 2019; Graboyes et al., 2020; Onyeador et al., 2020 |
Given the wide variation in frequency of specialties addressed, we explicitly avoid presenting conclusions that are specific to particular specialties. Our goal in reviewing these intervention strategies is to explore evidence-based strategies to counter the different ways implicit racial bias plays a role in the provision of healthcare. We hope that the application of these interventions contributes to a more equitable and effective healthcare system.
Individual Strategy #1: Awareness Intervention
Our review of implicit bias interventions in the healthcare domain identified eight (8) articles that specifically discussed the awareness intervention strategy. Awareness intervention strategies typically focus on empowering individuals to understand and acknowledge the role of implicit racial bias in healthcare, and, where applicable, in their provision of care to patients.
Across the articles the strategy is broken down into two steps:
Raising awareness about implicit bias itself.
Reflecting on one’s own implicit biases and how they might manifest within the professional environment.
The effectiveness of awareness intervention strategies can vary (Balakrishnan & Arjmand, 2019) based on a variety of factors (Alspach, 2018; Sukhera et al., 2018a). Healthcare research published between 2018-2020 and analyzed here concur that inclusion and intentional design of the second step, reflection, is essential to a more successful awareness intervention strategy (Alspach, 2018; Backhus et al., 2019; Motzkus et al., 2019). Specifically, scholars have empirically demonstrated that early interventions (e.g. year 1 of medical school) that include documenting reflections through writing (Avant & Gillespie, 2019; Motzkus et al., 2019), reflection upon an individual’s own culture and the extant culture of medicine they study/work in (White III et al., 2018), and sustained awareness intervention efforts (Backhus et al. 2019; see also Onyeador et al., 2020 and Alspach, 2018 for further rationales regarding longitudinal studies of impact) can have statistically significant impacts. Studies of this strategy involved professional students (Avant & Gillespie 2019; Motzkus et al., 2019; White et al. 2018) as well as medical residents and faculty (Sherman et al., 2019).
Individual Strategy #2: Adopt Evidence-Based Mitigation Strategies
Three (3) studies focus attention on practices providers should engage in consciously to thwart unconscious bias. Prior research indicated that practices like group-based debriefing could facilitate a transformation of how students reflect upon their experiences (Teal et al., 2010) and support those who feel less at ease in addressing race or ethnicity-related issues in group settings (Littleford et al., 2005; see also Burgess et al. 2019).
Among the “debiasing” strategies outlined for implicit bias mitigation, Balakrishnan and Arjmand (2019) specifically suggested perspective-taking and counter stereotypical examples as crucial factors in addressing implicit bias among healthcare providers. The authors maintained that implicit biases not only affect interactions between providers and patients but also influence the dynamics among providers themselves. A nursing education review by Narayan (2019) echoed this suggestion. Citing the advice from the Joint Commission, Narayan contended that healthcare providers should employ emotional regulation, partnership building, and perspective taking during clinical encounters to mitigate biases. Furthermore, alongside partnership building and perspective taking, the recommendations also included addressing bias through counter stereotypic imaging, individuation, enhancing opportunities for intergroup contact, and stereotype replacement.
Additionally, research on implicit bias intervention strategies expanded to incorporate an examination of different agents in the interactions affected by implicit bias. Moving away from a focus on providers, Bermudez (2018) applied social dreaming theory and the social dreaming matrix in group therapy settings. He argued that this approach provides a “container” for processing and healing racial trauma due to implicit bias. Focusing on the receivers' perspective, this psychoanalytic approach aims to a) address the impact of implicit bias on individuals, and b) facilitate their healing process in groups.
Individual Strategy #3: Design Interventions with Resistance in Mind
Research published in 2018-2020 cautioned against thinking that the awareness strategy is sufficient or without pitfalls (Backhus et al. 2019; Alspach 2018; Sukhera et al., 2018a). While awareness interventions can help participants uncover their own implicit biases, they can also trigger resistance and denial (Gonzalez et al., 2019). Our review identified five (5) articles that discussed these reactions and provided strategies and insights for mitigating potential negative responses to awareness interventions. Resistance manifests in various ways, including: questioning the validity of tests like IATs (Gatewood et al., 2019); anticipating negative emotions when acknowledging one’s own bias, especially when disclosing it publicly (Gonzalez et al., 2019); subtle discouragement of open discussion about implicit bias related to racial and ethnic subgroups (Gonzalez et al., 2019); and frustration stemming from the conflicts between one’s professional ideals and their susceptibility to implicit bias (Sukhera et al., 2018b).
The IAT can be used in distinct and complementary ways; curriculum designers and educators must consider the premise behind the test, and potential reactions from learners, and have a plan in place to address such reactions prior to delivering instruction. Gatewood and colleagues’ 2019 study of nursing students illustrated why clarity about the role and effectiveness of the IAT is instrumental in mitigation. Sukhera and colleagues (2018b) also affirmed the importance of IAT role clarity.
Although the evaluation of the session at the aggregated level was positive, some students expressed doubts regarding the legitimacy of the IAT test. Specifically, they raised doubts that the test appeared to have measured dexterity instead of bias. Gatewood and team (2019) acknowledged this skepticism and further substantiated this finding with similar concerns voiced in previous research (Gonzalez et al., 2014). These concerns may stem from a lack of full grasp of the IAT test’s critical design, particularly regarding the counterbalance for the order of two groupings of response targets. The main IAT question is which response mapping participants find easier to use, instead of simply assessing the error rate, which could be interpreted as a sign of dexterity. Gatewood et al. (2019) suggested that future studies should explore participants' confidence in the accuracy of the IAT and their ability to engage in self-reflection at different levels of learning.
Two qualitative studies looked at more individual-level responses to test results. Gonzalez et al.’s (2019) study of medical students and Sukhera et al.’s (2018b) study of medical faculty and residents both found shame and fear of public disclosure of implicit bias were barriers that fostered resistance to implicit bias instruction. Sukhera et al.’s study also revealed the dissonance. The study recruited 21 healthcare faculty and resident participants and had them take the IAT related to mental illness. Afterwards, participants were asked to draw a picture about their experience with the IAT. Using grounded theory, a methodology that involves the construction of hypotheses and theories through the collecting and analysis of data by inductive reasoning, the researchers analyzed the responses and found that the participants experienced tensions between an idealized professional identity that aspires to be unbiased and an actual identity that was susceptible to implicit bias. The participants described their process of reconciling these tensions, which involved acknowledging the existence of implicit bias while actively working towards self-improvement. To manage implicit bias, the participants emphasized the importance of relationships, including communicating their experiences with others and potentially seeking guidance from faculty mentors. Sukhera and colleagues (2018b) concluded that adopting a mindset of self-improvement while acknowledging personal limitations could serve as a model for addressing implicit bias among healthcare professionals. These strategies, combined with peer group discussion (see Sherman et al. 2019; Tsai & Michelson, 2020) may foster better uptake of mitigation efforts by anticipating and addressing resistance with intentionality up front.
Only an environment that avoids triggering defensiveness or denial can help an individual better process feedback received during awareness exercises, thereby effectively reducing implicit bias. Alspach (2018) emphasized that awareness exercises should be conducted in a non-threatening environment where one’s biases can be privately discovered. It is equally important to know that stereotyping is common for most of us. The articles associated with this strategy emphasize the importance of addressing potential resistance as a primary concern when designing and implementing awareness-based implicit bias intervention training.
Institutional Strategy #1: Incorporate Advances in Curriculum Development
Neither implicit racial biases nor attempts to address them function in a vacuum. Curriculum, whether formal or informal, plays a pivotal role in shaping students' awareness and their capacity to challenge their own biases. A variety of articles (7) from our review of literature from 2018 to 2020 were concerned with this theme. While relatively little is known about the percentage of medical education programs that have begun to implement these trainings and what their training curricula entail, Tsai and Michelson (2020) conducted one of the first studies aimed at answering these questions, using a nation-wide survey of 64 pediatric residency program directors. Their results revealed that 63% of the surveyed programs were already delivering some form of training to mitigate implicit bias. The survey respondents also identified a number of perceived barriers to implementation. Time constraints were often reported as the biggest challenge when adding more materials to an already intense program (Tsai & Michelson, 2020). These findings highlighted the need for more theoretically sound, evidence-based, and time efficient implicit bias intervention training models and curricula. From single course designs to more systematic intervention models for curriculum implementation, these articles explore diverse pieces of the puzzle, like strategies for screening vignettes used in curriculum materials and the factors impacting specific groups’ receptivity to a curriculum design.
Echoing van Ryn et al., (2015), Hernandez (2018), Burgess et al. (2019) and Motzkus et al. (2019) all found that medical students enter medical school and become habituated to norms and practices that can often reinforce rather than mitigate implicit racial bias, with serious implications for patient care. For example, Burgess and colleagues (2019) found lower levels of patient empathy among their strongly conservative respondents at the 4th year versus the 1st year of medical school, suggesting a role for medical school norms beyond individuals’ ideologies. Hernandez suggested leaders harness the opportunity to change institutional norms to mitigate implicit bias among students by assessing the formal and informal curricula, and the so called “hidden curriculum,” which are transmitted through structural and cultural factors such as methods of evaluation and colloquialisms.
Several studies focus attention on practices providers should engage in consciously to thwart unconscious racial bias. Bermudez (2018) applied social dreaming theory and the social dreaming matrix in sessions with students, faculty, and staff. In documenting his experiments from these psychotherapy workshops Bermudez concluded that the social dreaming matrix offered a distinctive chance for participants to perceive the struggles of others with implicit bias and racial trauma as if they were their own. Through this reflection and meaning creation process, a collective psychoanalytic path is formed, leading to an improved and proactive social and moral imagination that may intervene against the negative effects of implicit racial bias.
In a similar vein multiple studies (Burgess et al., 2019; Fadus et al., 2019; Stone et al., 2020) provided evidence that a tailored approach beyond the standard approach to race in curriculum and course design is important. In light of their findings, Burgess et al. (2019) suggests designing course content that resonates with more conservative individuals within curricula that might focus on values such as respect for authority and in-group loyalty and using influential figures in the medical profession as the source of communication. Fadus et al. (2019) suggests a nuanced approach that doesn’t rely solely on a patient’s appearance to infer racial or cultural identity but strives to obtain additional relevant information like cultural or immigrant backgrounds that help providers develop a comprehensive understanding of the factors that shape the values, attitudes and symptomatology among patients from diverse backgrounds. Specifically, the educational experience can raise awareness regarding common disparities by race that exist in healthcare settings, such as the disproportionate administration of higher doses of anti-psychotics to Black men that cannot be solely explained by clinical severity (Walkup et al., 2000). These curricular innovations aim to help medical students to grasp the implications of cognitive errors such as confirmation bias and framing, which may perpetuate misunderstanding of racial and ethnic minority patients.
Due to prevailing stereotypes that often characterize Hispanic/Latinx patients as medically noncompliant (Sabin et al., 2009), Jeff Stone and colleagues (2020) conducted a study comparing implicit racial bias levels of first-year medical students from different racial and ethnic backgrounds toward Hispanics before and after two active learning workshops. The workshops covered topics such as the psychological mechanisms of intergroup bias, and the effects of implicit bias on patient care. Then, the students completed a series of activities to learn how to control their implicit bias when interacting with patients. Prior to the workshops, assessment revealed that both the majority and nontarget minority groups held considerable levels of implicit stereotypes regarding Hispanics, but the target minority group did not. After completing the workshops, the majority group showed a significant decrease in implicit bias, but this change was not found in the nontarget minority group. The main findings from this study are two-fold. First, it showed that both proactive and reactive strategies are effective in mitigating implicit bias in medical students. According to Stone and colleagues (2020), activating beliefs or “stereotypes” to categorize patients can be helpful in diagnosing and treating patients using epidemiology and clinical case studies. Thus, as opposed to promoting a strategy focusing on negating automatic associations, it may be more effective to train medical students on proactive and reactive strategies to make the switch from category-based practice to individual-based processing when interacting with patients from stigmatized groups. The second contribution of this study was to demonstrate that not all ethnic and racial minority individuals respond the same way when learning to control implicit bias. This finding led to the recommendation highlighted by the authors that tailoring may be necessary in designing the materials and activities for implicit bias intervention curriculum. It involves not only customizing the context of the materials to match the scenarios and research findings to specific doctor-patient interactions, but also culturally tailoring the materials and activities for medical students of different ethnic and racial minority groups.
Institutional Strategy #2: Pilot Novel Curricula
Three (3) studies offered curricular interventions that can be piloted systematically at the department or school (e.g., medical school, nursing school, or pharmacy school) level. The ability of an individual to consistently adopt and uphold a trauma-informed approach is contingent upon their own well-being. For this reason, the studies discussed here acknowledge and incorporate individual strategy insights when designing their institutional strategy.
The Trauma-Informed Medical Education (TIME) model was proposed to foster awareness that medical students and trainees can experience trauma from an environment imbued with implicit bias and to advocate for new practices in medical education. Authors Aneesa McClinton and Cato Laurencin (2020) argued that the prevalence of implicit bias in patient-provider interactions and its impact on learners’ experiences (see, e.g., Green 2018; Backhus et al. 2018; Capers et al. 2017; Rodriguez et al. 2014) necessitates a set of curricular principles aimed at establishing a supportive environment (Ravi & Little, 2017). Since identifying individuals who have experienced trauma can be challenging in the context of institutions, trauma-informed principles can be implemented as a universal precautionary measure (see also Kuehn, 2020). In so doing, the TIME approach does not rely on individual disclosures of the specific trauma endured (therefore avoiding privacy policy issues). Instead, it operates on a set of principles aimed at establishing a supportive environment (Ravi & Little, 2017). Similar to Stone et al.’s (2020) attention to proactive and reactive strategies used in clinical settings, the TIME model proposes four Rs for medical student training in implicit bias mitigation at both the individual and institutional levels: realize, recognize, respond and resist (McClinton & Laurencin, 2020).
While the TIME model has focused on medical students and trainees, the Health Equity Rounds (HER) model is aimed at faculty and practitioners across various training levels and disciplines engaging in conversations about how racism and implicit bias directly affect patient care. Joanna Perdomo and colleagues (2019) developed HER in a pediatrics department and empowered medical residents to design and later advise on curriculum development. Participants in this longitudinal, case-based curriculum included attending physicians, fellows, residents, and medical students from departments such as pediatrics and family medicine. HER sessions were held quarterly during dedicated time for departmental case conferences. Incorporating the curriculum into regularly offered case conferences can address a concern about fitting implicit racial bias into a crowded curriculum (Tsai & Michaelson 2020). The cases used in HER sessions were selected from real provider-patient interaction scenarios submitted by residents and faculty. In addition to a wide coverage of topics spanning from contraceptive counseling to Williams syndrome, these cases were also curated to focus on issues connected to implicit bias and racism to foster interdisciplinary, cross-rank conversations instead of complex medical details that might create barriers to understanding. The authors employed a variety of evidence based individual strategy techniques to enhance case presentation, including perspective taking and individuation practice based on imagery exercises. Moreover, the curriculum incorporated different methods, including reflection essays, share out loud, and think-pair-share, to encourage the participants to practice the learned techniques. Survey feedback about HER sessions indicated that HER helped them gain awareness, motivation, and tools to reflect on their implicit biases, which subsequently benefited their clinical practices. Their findings also echoed some findings we discussed at the individual level, suggesting that tailored approaches could be combined with HER curriculum for maximal impact.
Third and finally, Billy Thomas and Amber Booth-McCoy (2020) proposed a theoretical model for reducing the impact of implicit bias with descriptions of eight longitudinal stages. The first six stages include: 1) awareness of implicit biases, 2) an increase in knowledge about the science of implicit bias, 3) acknowledgement and acceptance of implicit biases and their effect on behavior and patient outcomes, 4) intentional behavioral change by self-reflection and perspective taking, 5) direct application of strategies promoting behavioral changes, 6) affirmation of behavioral change through positive feedback. These six process stages are thought to lead to a pair of final result stages: 7) actual mitigation of implicit biases through behavioral change and 8) improved patient-provider relationships and better health outcomes and equity. Along with this theoretical model, Thomas and Booth-McCoy (2020) also reviewed four intervention strategies and their outcomes. They suggested that medical schools should adopt mandatory implicit association tests and provide cultural humility training as a curriculum change. In this way, medical students can learn to care for minority and underserved communities through experience.
Institutional Strategy 3: Adopt a Nuanced Institutional Approach to Structural Racism
Just as patients should not be treated as if race is a one-size-fits-all shaper of health outcomes, neither should providers or students be assumed to benefit from one-size-fits-all training (see also Burgess et al. 2019). Similarly, while structural racism is pervasive it does not operate uniformly or identically in all contexts.
Several articles acknowledged small but persistent effects among factors that could be assumed to play a bigger role. Moving protocols away from emphasizing implicit bias training in isolation can provide additional impact on reducing racial disparities. An equitable and effective healthcare environment can be constructed at multiple layers, including incorporating counter stereotypical examples in educational materials, enhancing interracial contact in the physical environment through diversifying the rank of faculty and tapping into the racial and socioeconomic diversity of the city where the medical institute is embedded.
Acculturation should also be a part of medical curricular design (including additional education and training in interview skills) to ensure that students and trainees are using unbiased instruments in an unbiased way, ultimately contributing to a more equitable and effective treatment. For example, Fadus et al. (2019) suggested that psychiatric providers enhance their culturally informed interview techniques, utilize existing tools with cultural sensitivity (see also Lewis-Fernández et al., 2020) and improve their structural competency to better recognize the implications of socioeconomic factors on psychiatric disorder symptoms. In a similar vein, Quinn Capers and colleagues (2020) also emphasized the importance of real patient interactions in medical education. They proposed that teaching hospitals should encourage regularly recurring gatherings of health providers to review incidents in which bias or racism is suspected to have occurred.
Residency interviews are another hurdle where implicit racial bias can manifest itself (Backhus et al., 2019). This analysis referenced a study indicating that a large proportion of medical students encounter potentially discriminatory questions during their residency match interviews (Santen et al., 2010). Backhus et al. (2019) suggested that one way to mitigate this issue is to design standardized interview questions tailored to what trainees may experience at the residency program, rather than utilizing unstructured interview formats. The authors also noted that implementing a scoring system to evaluate the interviewee's responses to these questions could further enhance the standardized interview process's effectiveness. The collective evidence presented by Backhus and colleagues (2019) emphasized the need for establishing initiatives at the institutional level to address implicit racial bias in admission and enhancing support for minority faculty members in academic medicine, thereby fostering the growth of minority medical students.
At the institutional level of implicit bias mitigation, Ivuoma Onyeador and colleagues (2020) examined the influence of three medical school factors, including interracial contact, medical school environment, and diversity training (for both implicit and explicit racial bias) during medical residency. Using a 6-year longitudinal dataset, they found that the quality of contact predicted a very small but consistent reduction in implicit bias. However, racial climate, modeling of bias, and length of diversity training did not consistently lower implicit bias. These results provided valuable insight into the long-term effects of implicit bias mitigation trainings in medical education and highlighted the importance of encouraging interracial contact at the institutional level.
Healthcare continues to present unique opportunities for evidence-based research to mitigate implicit racial biases. For example, implicit bias can influence how medical practitioners allocate healthcare resources, potentially contributing to disparities among patients of different racial and ethnic backgrounds. Evan Graboyes and colleagues (2020) discussed strategies to address this issue in head and neck cancer care delivery, specifically in how surgical cases are prioritized. Previously, it has been suggested that a "color-blind" decision-aid prioritization system, which excludes race information from the decision-making process, could help rectify unequal treatment of racial and ethnic minority patients. Graboyes et al. (2020) cautioned against this simplistic approach because, even after removing race/ethnicity data, clinical stage and comorbidity severity would still have a role in this prioritization scheme. As African American and Hispanic/Latino patients are more likely to have comorbidities and present with advanced stages of diseases, implementing a decision-aid prioritization system solely focused on maximizing benefits based on comorbidity and disease stage could inadvertently perpetuate bias against these patients. Therefore, a comprehensive approach is necessary to mitigate bias and ensure equitable treatment for all patients. Graboyes and colleagues suggested a possible solution to this problem, which is developing a prioritization scheme that incorporates evidence-based, data-driven weights based on patient populations and local or regional prevalence of the relevant diseases. Another solution could be to develop a framework that prioritizes racial and ethnic minorities based on ethical principles, such as giving priority to those who are worse off (Graboyes et al., 2020). Although the optimal solution has yet to be determined, Graboyes and colleagues’ discussion emphasized the need for objective and metric-based decision aid/intervention tools to address disparities associated with implicit racial biases. Graboyes and colleagues’ recommendation for such tools concurs with findings in the 2018 Sate of the Science. Hymel et al. (2018) recommended that future attention needs to be devoted to developing validated and evidence based AHT screening tools in order to reduce the potential negative impact of implicit racial and ethnic bias in AHT diagnosis and evaluation.
While many authors in our three-year dataset focused on infant and pediatric contexts, one publication stood out for its development of a novel end-of-life tool. Elizabeth Chuang and colleagues (2020) developed a novel tool on the basis of the Race IAT to measure provider’s implicit bias in end-of-life (EOL) care. Through literature review, the researchers identified an initial pool of words used in EOL care that fit under two categories: comfort-oriented or aggressive. Clinicians in the specialties that treat serious illness were invited to rate and rank the words included in the initial pool. Words that were consistently sorted and ranked as representative of the two target categories were chosen as attributes in the novel EOL-IAT. Participants were instructed to categorize these words with two response keys, representing counterbalanced pairings of race (Black/White) and attributes (comfort/aggressive). This tool was piloted online through ProjectImplicit® and yielded promising results for practical application. This study represented an effort in customizing tools for accessing implicit biases held by providers of different specialties. It serves as a reminder for us that providers' implicit bias may not be as straightforward as associating White people with the attribute of "good" and
Black people with “bad”. Instead, it can manifest in ways specific to the care of the specialty. For example, in EOL care, it may be more critical to determine if providers tend to associate White patients with the attribute of “comfort”, while exhibiting a stronger tendency to associate “aggressive” with Black patients.
Conclusion & Directions for Future Research
Conclusion & Directions for Future ResearchFrom racial disparities in specific areas of patient care and the repercussions of the COVID-19 pandemic, to the unfair interactions among providers as well as among medical students themselves, 61 articles published over a three-year period between 2018 and 2020 documented the tangible consequences of these biases. While acknowledging the existence of the issues posed by implicit bias is a start, effectively addressing it in the field of healthcare requires actionable and diverse strategies. Emerging research findings from our review underscored the need for intervention methods that combine the best of what we know at the individual level about how to mitigate the impact of implicit racial bias with evidence-based institutional interventions tailored to the diverse population of healthcare providers and trainees. Moreover, it continues to be necessary to develop a deeper understanding of how implicit bias operates at the individual and institutional levels. The healthcare domain’s collective commitment to dismantling these biases is vital, as it enhances the chance of every patient receiving unbiased and compassionate care, while also affording equitable opportunities to those providing services in the healthcare system. If 2020 taught us anything, it is that no country or community can be completely isolated from the healthcare challenges faced by others.
Even though decades of implicit racial bias research have continued to confirm the negative impact of bias in 2018-2020 there remain areas where research conclusions are unsettled, providing new directions for research. Sukhera et al.’s (2018a) review of healthcare education studies that use the IAT found that the IAT is often used in two ways: as a metric to evaluate the success of an educational activity or as a tool to promote awareness while triggering discussion and reflection. The IAT can be used in distinct and complementary ways; curriculum designers and educators must consider the premise for using the test, anticipate potential reactions from learners, and have a plan in place to address such reactions prior to delivering instruction. For example, when the goal of implicit bias intervention is to improve provider communication behaviors, Hagiwara et al., (2019) raised concerns about the limitations of the existing patient provider communication coding systems, such as the Roter Interaction Analysis System (RIAS) and the Four Habits Coding Scheme. They noted that these systems fail to consistently include an assessment of nonverbal or paraverbal behaviors, which are often associated with the manifestation of implicit bias. To address these shortcomings, the authors recommended that more research should be aimed towards identifying specific provider communication behaviors that may reflect provider implicit racial bias, with a special focus of integrating minority patient perspectives. By gathering narratives from minority patients, researchers can identify nonverbal and paraverbal cues that are consistent with implicit racial bias and then develop coding systems to recognize discrete and quantifiable communications for providers to address.
Notably, Maina et al.’s 2018 review indicated that the research on the impact of providers’ implicit bias on patient care and outcomes had mixed results. When it comes to mitigation efforts, their review found only two intervention studies that investigated methods to reduce implicit bias among healthcare providers, with only one study demonstrating a post-intervention reduction in implicit bias. The authors also highlighted several limitations among the reviewed studies, including the use of convenience samples, low response rates, overreliance on vignettes instead of real-world measures, limited ability to infer causality due to cross-sectional study designs, and an excessive focus on physicians’ implicit racial bias rather than that of other types of healthcare providers. While the latter limitation has been addressed by multiple studies in our dataset, the opportunities for both empirical (additional evidence-based findings) and methodological innovations (development of more precise and successful tools to study implicit racial bias) in this line of scholarship remain. We hope these areas for future research will be addressed across many healthcare specialties, reducing disparities and producing better medical outcomes in the years to come.
References
ReferencesAbelson, J. S., Symer, M. M., Yeo, H. L., Butler, P. D., Dolan, P. T., Moo, T. A., & Watkins, A. C. (2018). Surgical time out: Our counts are still short on racial diversity in academic surgery. American journal of surgery, 215(4), 542–548. https://doi.org/10.1016/j.amjsurg.2017.06.028
Al-Quran, F. A., Al-Ghalayini, R. F., & Al-Zu'bi, B. N. (2011). Single-tooth replacement: factors affecting different prosthetic treatment modalities. BMC oral health, 11, Article 34. https://doi.org/10.1186/1472-6831-11-34
Alspach, J. G. (2018). Implicit bias in patient care: An endemic blight on quality care. Critical Care Nurse, 38(4), 12-16. https://doi.org/10.4037/ccn2018698
Anderson, K. O., Green, C. R., & Payne, R. (2009). Racial and ethnic disparities in pain: Causes and consequences of unequal care. The journal of pain, 10(12), 1187-1204.
Avant, N. D., Gillespie, G. L., (2019). Pushing for health equity through structural competency and implicit bias education: A qualitative evaluation of a racial and ethnic health disparities elective course for pharmacy learners. Currents in Pharmacy Teaching and Learning, 11(4), 382-393. https://doi.org/10.1016/j.cptl.2019.01.013.
Backhus, L. M., Lui, N. S., Cooke, D. T., Bush, E. L., Enumah, Z., & Higgins, R. (2019). Unconscious bias: Addressing the hidden impact on surgical education. Thoracic surgery clinics, 29(3), 259–267. https://doi.org/10.1016/j.thorsurg.2019.03.004
Balakrishnan, K., & Arjmand, E. M. (2019). The impact of cognitive and implicit bias on patient safety and quality. Otolaryngologic clinics of North America, 52(1), 35–46.
Bermudez, G. (2018). The social dreaming matrix as a container for the processing of implicit racial bias and collective racial trauma. International Journal of Group Psychotherapy,
68(4), 538-560. https://doi.org/10.1080/00207284.2018.1469957
Bonica, A., Rosenthal, H., Blackwood, K., & Rothman, D. J. (2020). Ideological sorting of physicians in both geography and the workplace. Journal of Health Politics, Policy and Law, 45(6), 1023–1057. https://doi.org/10.1215/03616878-8641555
Bunik, M., Gao, D., & Moore, L. (2006). An investigation of the field trip model as a method for teaching breastfeeding to pediatric residents. Journal of Human Lactation, 22(2), 195–
Burgess, D. J., Hardeman, R. R., Burke, S. E., Cunningham, B. A., Dovidio, J. F., Nelson, D. B., Perry, S. P., Phelan, S. M., Yeazel, M. W., Herrin, J., & van Ryn, M. (2019). Incoming medical students' political orientation affects outcomes related to care of marginalized groups: Results from the medical student CHANGES study. Journal of Health Politics, Policy and Law, 44(1), 113–146. https://doi.org/10.1215/03616878-7206755
Burgess, D. J., Phelan, S., Workman, M., Hagel, E., Nelson, D. B., Fu, S. S., ... & Van Ryn, M. (2014). The effect of cognitive load and patient race on physicians' decisions to prescribe opioids for chronic low back pain: A randomized trial. Pain Medicine, 15(6), 965-974.
Cameron, M., & Guterman, N. B. (2007). Diagnosing conduct problems of children and adolescents in residential treatment. Child and Youth Care Forum, 36(1), 1–10. https://doi.org/10.1007/s10566-006-9027-6
Campbell, C. M., & Edwards, R. R. (2012). Ethnic differences in pain and pain management.
Pain management, 2(3), 219-230. https://doi.org/10.2217/pmt.12.7
Capers, Q. IV., Bond, D. A., & Nori, U. S. (2020). Bias and racism teaching rounds at an academic medical center. Chest, 158(6), 2688-2694.
Chae, D. H., Nuru-Jeter, A. M., Adler, N. E., Brody, G. H., Lin, J., Blackburn, E. H., & Epel, E. S. (2014). Discrimination, racial bias, and telomere length in African-American men.
American Journal of Preventive Medicine, 46(2), 103-111.
Chan, S., Kang, J., Bastron, B. Inaugural state of hate report: From pain to power. Last accessed January 8, 2024.
Chapman, E. N., Kaatz, A., & Carnes, M. (2013). Physicians and implicit bias: How doctors may unwittingly perpetuate health care disparities. Journal of general internal medicine,
Charleston, L. IV., & Spears, R. C. (2020). Equity of African American men in headache in the United States: A perspective from African American headache medicine specialists (part 2). Headache: The Journal of Head and Face Pain, 60(10), 2486-2494.
Chuang, E., Gong, M., Elk, R., & Cha, C. (2020). Development of a novel implicit association test for racial bias in end-of-life care—The EOL-IAT (RP304). Journal of Pain and Symptom Management, 60(1), 201-202.
Clark, E. Jr. (2007). Conduct disorders in African American adolescent males: The perceptions that lead to overdiagnosis and placement in special programs. Alabama Counseling Association Journal, 33(2), 1–7.
Cleveland Manchanda, E. C., & Macias-Konstantopoulos, W. L. (2020). Tackling gender and racial bias in academic emergency medicine: The perceived role of implicit bias in faculty development. Cureus, 12(11), Article e11325. https://doi.org/10.7759/cureus.11325
Coker, T. R., Elliott, M. N., Toomey, S. L., Schwebel, D. C., Cuccaro, P., Tortolero Emery, S., Davies, S. L., Visser, S. N., & Schuster, M. A. (2016). Racial and ethnic disparities in ADHD diagnosis and treatment. PEDIATRICS, 138(3), e20160407–e20160407. https://doi.org/10.1542/peds.2016-0407
Cooper, L. A., Roter, D. L., Carson, K. A., Beach, M. C., Sabin, J. A., Greenwald, A. G., & Inui, T. S. (2012). The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. American Journal of Public Health, 102(5), 979-987. http://doi.org/10.2105/AJPH.2011.300558
Crandlemire, L. A. (2020). Unconscious bias and the impacts on caring: The role of the clinical nursing instructor. International Journal for Human Caring, 24(2), 84-91.
Darling-Hammond, S., Michaels, E. K., Allen, A. M., Chae, D. H., Thomas, M. D., Nguyen, T. T., ... & Johnson, R. C. (2020). After “the China virus” went viral: Racially charged coronavirus coverage and trends in bias against Asian Americans. Health Education & Behavior, 47(6), 870-879. https://doi.org/10.1177/1090198120957949
Davis-Martin, R. (2020). Unique healthcare–related anxiety in the time of racial injustice and COVID. Families, Systems, & Health, 38(Suppl 1), 28–29.
Dyrbye, L., Herrin, J., West, C. P., Wittlin, N. M., Dovidio, J. F., Hardeman, R., Burke, S. E., Phelan, S., Onyeador, I. N., Cunningham, B., & van Ryn, M. (2019). Association of racial bias with burnout among resident physicians. JAMA Network Open, 2(7), Article e197457. https://doi.org/10.1001/jamanetworkopen.2019.7457
Fadus, M. C., Ginsburg, K. R., Sobowale, K., Halliday-Boykins, C. A., Bryant, B. E., Gray, K.
M., & Squeglia, L. M. (2020). Unconscious bias and the diagnosis of disruptive behavior disorders and ADHD in African American and Hispanic youth. Academic Psychiatry,
Fadus, M. C., Odunsi, O. T., & Squeglia, L. M. (2019). Race, ethnicity, and culture in the medical record: implicit bias or patient advocacy?. Academic Psychiatry, 43, 532-536.
Feisthamel, K. P., & Schwartz, R. C. (2009). Differences in mental health counselors’ diagnoses based on client race: An investigation of adjustment, childhood, and substance-related disorders. Journal of Mental Health Counseling, 31(1), 47–59. https://doi.org/10.17744/mehc.31.1.u82021637276wv1k
FitzGerald, C., & Hurst, S. (2017). Implicit bias in healthcare professionals: A systematic review.
Gatewood, E., Broholm, C., Herman, J., & Yingling, C. (2019). Making the invisible visible: Implementing an implicit bias activity in nursing education. Journal of Professional Nursing, 35(6), 447-451. https://doi.org/10.1016/j.profnurs.2019.03.004.
Gonzalez, C. M., Deno, M. L., Kintzer, E., et al. (2019). A qualitative study of New York medical student views on implicit bias instruction: Implications for curriculum development. Journal of General Internal Medicine, 34(4), 692–698. https://doi.org/10.1007/s11606019-04891-1
Gonzalez, C. M., Kim, M. Y., & Marantz, P. R. (2014). Implicit bias and its relation to health disparities: A teaching program and survey of medical students. Teaching and Learning in Medicine, 26(1), 64-71. https://doi.org/10.1080/10401334.2013.857341
Goodwin, M. (2018). Revisiting death: Implicit bias and the case of Jahi McMath. Hastings
Center Report, 48(S4), 77-80. https://doi.org/10.1002/hast.963
Graboyes, E., Cramer, J., Balakrishnan, K., Cognetti, D. M., López‐Cevallos, D., de Almeida, J. R., ... & Brenner, M. J. (2020). COVID‐19 pandemic and health care disparities in head and neck cancer: Scanning the horizon. Head & neck, 42(7), 1555-1559.
Green, C. R., Anderson, K. O., Baker, T. A., Campbell, L. C., Decker, S., Fillingim, R. B., ... & Vallerand, A. H. (2003). The unequal burden of pain: Confronting racial and ethnic disparities in pain. Pain medicine, 4(3), 277-294. https://doi.org/10.1046/j.1526https://doi.org/10.1046/j.1526-4637.2003.03034.x4637.2003.03034.x
Greene, J., Hibbard, J. H., & Sacks, R. M. (2018). Does the race/ethnicity or gender of a physician's name impact patient selection of the physician?. Journal of the National Medical Association, 110(3), 206-211. https://doi.org/10.1016/j.jnma.2017.05.010
Hagiwara, N., Dovidio, J. F., Stone, J., & Penner, L. A. (2020). Applied racial and ethnic healthcare disparities research using implicit measures. Social cognition, 38(Suppl), S68-S97. https://doi.org/10.1521/soco.2020.38.supp.s68
Hagiwara, N., Lafata, J. E., Mezuk, B., Vrana, S. R., & Fetters, M. D. (2019). Detecting implicit racial bias in provider communication behaviors to reduce disparities in healthcare:
challenges, solutions, and future directions for provider communication training. Patient education and counseling, 102(9), 1738-1743. https://doi.org/10.1016/j.pec.2019.04.023
Haider, A. H., Sexton, J., Sriram, N., Cooper, L. A., Efron, D. T., Swoboda, S., ... & Cornwell, E. E. (2011). Association of unconscious race and social class bias with vignette-based clinical assessments by medical students. JAMA, 306(9), 942-951.
Haider, A. H., Schneider, E. B., Sriram, N., Scott, V. K., Swoboda, S. M., Zogg, C. K., ... & Cooper, L. A. (2015). Unconscious race and class biases among registered nurses: vignette-based study using implicit association testing. Journal of the American College of Surgeons, 220(6), 1077-1086. https://doi.org/10.1016/j.jamcollsurg.2015.01.065
Hall, W. J., Chapman, M. V., Lee, K. M., Merino, Y. M., Thomas, T. W., Payne, B. K., ... & Coyne-Beasley, T. (2015). Implicit racial and ethnic bias among health care professionals and its influence on health care outcomes: A systematic review. American Journal of Public Health, 105(12), 60-76. https://doi.org/10.2105/AJPH.2015.302903
Hernandez, R. (2018). Medical students' implicit bias and the communication of norms in medical education. Teaching and Learning in Medicine, 30(1), 112-117.
Hymel, K. P., Laskey, A. L., Crowell, K. R., Wang, M., Armijo-Garcia, V., Frazier, T. N., ... & Karst, W. A. (2018). Racial and ethnic disparities and bias in the evaluation and reporting of abusive head trauma. The Journal of Pediatrics, 198, 137-143.
James, D. J., & Glaze, L. E., (2006). Mental health problems of prison and jail inmates (NCJ 213600). Bureau of Justice Statistics, Office of Justice Programs.
Jaryszak, E. M., Lander, L., Patel, A. K., Choi, S. S., & Shah, R. K. (2011). Prolonged recovery after out-patient pediatric adenotonsillectomy. International Journal of Pediatric Otorhinolaryngology, 75(4), 585-588. https://doi.org/10.1016/j.ijporl.2011.01.024
Johnson, T. J. (2020). Racial bias and its impact on children and adolescents. Pediatric Clinics,
67(2), 425-436. https://doi.org/10.1016/j.pcl.2019.12.011
Johnson, T. J., Hickey, R. W., Switzer, G. E., Miller, E., Winger, D. G., Nguyen, M., Saladino, R. A., & Hausmann, L. R. M. (2016). The impact of cognitive stressors in the emergency department on physician implicit racial bias. Academic Emergency Medicine, 23(3), 297305. https://doi.org/10.1111/acem.12901
Kuehn, B. M. (2020). Trauma-informed care may ease patient fear, clinician burnout. JAMA, 323(7), 595-597. https://doi.org/10.1001/jama.2020.0052
Lewis-Fernández, R., Aggarwal, N. K., & Kirmayer, L. J. (2020). The cultural formulation interview: Progress to date and future directions. Transcultural Psychiatry, 57(4), 487–496. https://doi.org/10.1177/1363461520938273
Littleford, L. N., Wright, M. O., & Sayoc-Parial, M. (2005). White students' intergroup anxiety during same-race and interracial interactions: A multimethod approach. Basic and
Applied Social Psychology, 27(1), 85–94. https://doi.org/10.1207/s15324834basp2701_9
Lowe, C. L., Beach, M. C., & Roter, D. L. (2020a). Genetic counselor implicit bias and its effects on cognitive and affective exchanges in racially discordant simulations. Journal of Genetic Counseling, 29(3), 332-341. https://doi.org/10.1002/jgc4.1243
Lowe, C., Beach, M. C., & Roter, D. L. (2020b). Individuation and implicit racial bias in genetic counseling communication. Patient Education and Counseling, 103(4), 804-810. https://doi.org/10.1016/j.pec.2019.10.016
Ly, D. P., Seabury, S. A., & Jena, A. B. (2016). Differences in incomes of physicians in the United States by race and sex: observational study. BMJ, 353, Article i2923.
Maina, I. W., Belton, T. D., Ginzberg, S., Singh, A., & Johnson, T. J. (2018). A decade of studying implicit racial and ethnic bias in healthcare providers using the implicit association test. Social Science & Medicine, 199, 219-229.
Manchanda, E. C. C., & Macias-Konstantopoulos, W. L. (2020). Tackling gender and racial bias in academic emergency medicine: the perceived role of implicit bias in faculty development. Cureus, 12(11), Article e11325. https://doi.org/10.7759/cureus.11325
Maxfield, C. M., Thorpe, M. P., Desser, T. S., Heitkamp, D., Hull, N. C., Johnson, K. S., ... & Grimm, L. J. (2020). Awareness of implicit bias mitigates discrimination in radiology resident selection. Medical Education, 54(7), 637-642.
McClinton, A., & Laurencin, C. T. (2020). Just in TIME: Trauma-informed medical education.
Journal of Racial and Ethnic Health Disparities, 7(6), 1046-1052.
Merino, Y., Adams, L., & Hall, W. J. (2018). Implicit bias and mental health professionals:
Priorities and directions for research. Psychiatric Services, 69(6), 723-725.
Miller, M. M., Williams, A. E., Zapolski, T. C., Rand, K. L., & Hirsh, A. T. (2020). Assessment and treatment recommendations for pediatric pain: The influence of patient race, patient
gender, and provider pain-related attitudes. The Journal of Pain, 21(1-2), 225-237.
Mizock, L., & Harkins, D. (2011). Diagnostic bias and conduct disorder: Improving culturally sensitive diagnosis. Child & Youth Services, 32(3), 243–253. https://doi.org/10.1080/0145935X.2011.605315
Moskowitz, G. B., Stone, J., & Childs, A. (2012). Implicit stereotyping and medical decisions:
Unconscious stereotype activation in practitioners' thoughts about African Americans.
American Journal of Public Health, 102(5), 996-1001.
Motzkus, C., Wells, R. J., Wang, X., Chimienti, S., Plummer, D., Sabin, J., et al. (2019). Preclinical medical student reflections on implicit bias: Implications for learning and teaching. PLoS ONE, 14(11), Article e0225058.
Muntinga, M., Beuken, J., Gijs, L., & Verdonk, P. (2020). Are all LGBTQI+ patients White and male? Good practices and curriculum gaps in sexual and gender minority health issues in a Dutch medical curriculum. GMS Journal of Medical Education, 37(2), Article Doc22.
Narayan M. C. (2019). CE: Addressing Implicit Bias in Nursing: A Review. The American journal of nursing, 119(7), 36–43. https://doi.org/10.1097/01.NAJ.0000569340.27659.5a
Nelson A. (2002). Unequal treatment: Confronting racial and ethnic disparities in health care. Journal of the National Medical Association, 94(8), 666–668.
Nosek, B. A., Bar-Anan, Y., Sriram, N., Axt, J., & Greenwald, A. G. (2014). Understanding and using the brief Implicit Association Test: Recommended scoring procedures. PLoS ONE,
9(12), Article e110938. https://doi.org/10.1371/journal.pone.0110938
Onyeador, I. N., Wittlin, N. M., Burke, S. E., Dovidio, J. F., Perry, S. P., Hardeman, R. R., ... & van Ryn, M. (2020). The value of interracial contact for reducing anti-black bias among non-black physicians: A cognitive habits and growth evaluation (CHANGE) study report. Psychological Science, 31(1), 18-30. https://doi.org/10.1177/0956797619879139
Pate, J. T., Blount, R. L., Cohen, L. L., & Smith, A. J. (1996). Childhood medical experience and temperament as predictors of adult functioning in medical situations. Children's Health Care, 25(4), 281-298. https://doi.org/10.1207/s15326888chc2504_4
Patel, N., Patel, S., Cotti, E., Bardini, G., & Mannocci, F. (2019). unconscious racial bias may affect dentists’ clinical decisions on tooth restorability: A randomized clinical trial. JDR Clinical & Translational Research, 4(1), 19-28. https://doi.org/10.1177/2380084418812886
Penner, L. A., Dovidio, J. F., Gonzalez, R., Albrecht, T. L., Chapman, R., Foster, T., Harper, F. W. K., Hagiwara, N., Hamel, L. M., Shields, A. F., Gadgeel, S., & Simon, M. S. (2016). The effects of oncologist implicit racial bias in racially discordant oncology interactions.
Journal of Clinical Oncology, 34(24), 2874-2880.
Perdomo, J., Tolliver, D., Hsu, H., He, Y., Nash, K. A., Donatelli, S., ... Michelson, C. D. (2019). Health Equity Rounds: An interdisciplinary case conference to address implicit bias and structural racism for faculty and trainees. MedEdPORTAL, 15, Article 10858.
Pereda, B., & Montoya, M. (2018). Addressing implicit bias to improve cross-cultural care. Clinical Obstetrics and Gynecology, 61(1), 2-9. https://doi.org/10.1097/GRF.0000000000000341
Peterson, C., Xu, L., Florence, C., & Parks, S. E. (2015). Annual cost of U.S. hospital visits for pediatric abusive head trauma. Child Maltreatment, 20(3), 162–169.
Plaisime, M. V., Malebranche, D. J., Davis, A. L., & Taylor, J. A. (2017). Healthcare providers’ formative experiences with race and Black male patients in urban hospital environments.
Journal of Racial and Ethnic Health Disparities, 4, 1120–1127.
Polsky, D., & Weiner, J. (2015). The Skinny on Narrow Networks in Health Insurance Marketplace Plans. The Leonard Davis Institute of Health Economics.
https://d197nivf0nbma8.cloudfront.net/uploads/archive/pdf/the-skinny-on-narrowhttps://d197nivf0nbma8.cloudfront.net/uploads/archive/pdf/the-skinny-on-narrow-networks.pdfnetworks.pdf
Ravi, A., & Little, V. (2017). Providing trauma-informed care. American Family Physician, 95(10), 655-657.
Reece, R. M., & Sege, R. (2000). Childhood head injuries: Accidental or inflicted?. Archives of Pediatrics & Adolescent Medicine, 154(1), 11–15.
Rodriguez, J. E., Campbell, K. M., Fogarty, J. P., & Williams, R. L. (2014). Underrepresented minority faculty in academic medicine: A systematic review of URM faculty development. Family medicine, 46(2), 100–104.
Sabin, J., Nosek, B. A., Greenwald, A., & Rivara, F. P. (2009). Physicians' implicit and explicit attitudes about race by MD race, ethnicity, and gender. Journal of Health Care for the Poor and Underserved, 20(3), 896–913. https://doi.org/10.1353/hpu.0.0185
Santen, S. A., Davis, K. R., Brady, D. W., & Hemphill, R. R. (2010). Potentially discriminatory questions during residency interviews: Frequency and effects on residents' ranking of programs in the national resident matching program. Journal of Graduate Medical Education, 2(3), 336–340. https://doi.org/10.4300/JGME-D-10-00041.1
Saunders, W., & Saunders, E. (1998). Prevalence of periradicular periodontitis associated with crowned teeth in an adult Scottish subpopulation. British Dental Journal, 185(3), 137– 140. https://doi.org/10.1038/sj.bdj.4809750
Schultz, P. L., & Baker, J. (2017). Teaching strategies to increase nursing student acceptance and management of unconscious bias. Journal of Nursing Education, 56(11), 692-696. https://doi.org/10.3928/01484834-20171020-11
Shapiro, N., Wachtel, E. V., Bailey, S. M., & Espiritu, M. M. (2018). Implicit physician biases in periviability counseling. The Journal of pediatrics, 197, 109-115.
Sherman, M. D., Ricco, J., Nelson, S. C., Nezhad, S. J., & Prasad, S. (2019). Implicit bias training in a residency program: Aiming for enduring effects. Family Medicine, 51(8),
Snowden, L. R. (2003). Bias in mental health assessment and intervention: Theory and evidence.
American Journal of Public Health, 93(2), 239-243.
Stewart, M., Brown, J. B., Weston, W., McWhinney, I. R., McWilliam, C. L., & Freeman, T.
(2013). Patient-centered medicine: Transforming the clinical method. CRC press.
Stone, J., & Moskowitz, G. B. (2011). Non‐conscious bias in medical decision making: What can be done to reduce it?. Medical Education, 45(8), 768-776. https://doi.org/10.1111/j.1365https://doi.org/10.1111/j.1365-2923.2011.04026.x2923.2011.04026.x
Stone, J., Moskowitz, G. B., Zestcott, C. A., & Wolsiefer, K. J. (2020). Testing active learning workshops for reducing implicit stereotyping of Hispanics by majority and minority group medical students. Stigma and Health, 5(1), 94-103.
Street Jr, R. L., Makoul, G., Arora, N. K., & Epstein, R. M. (2009). How does communication heal? Pathways linking clinician–patient communication to health outcomes. Patient
Education and Counseling, 74(3), 295-301. https://doi.org/10.1016/j.pec.2008.11.015
Sukhera, J., Milne, A., Teunissen, P. W., Lingard, L., & Watling, C. (2018a). Adaptive reinventing: Implicit bias and the co-construction of social change. Advances in Health Sciences Education, 23, 587-599. https://doi.org/10.1007/s10459-018-9816-3
Sukhera, J., Wodzinski, M., Teunissen, P. W., Lingard, L., & Watling, C. (2018b). Striving while accepting: Exploring the relationship between identity and implicit bias recognition and management. Academic Medicine, 93(11S), 82-88.
Tait, R. C., & Chibnall, J. T. (2014). Racial and ethnic disparities in the assessment and treatment of pain: Psychosocial perspectives. American Psychologist, 69(2), 131–141.
Tajeu, G. S., Halanych, J., Juarez, L., Stone, J., Stepanikova, I., Green, A., & Cherrington, A. L. (2018). Exploring the association of healthcare worker race and occupation with implicit and explicit racial bias. Journal of the National Medical Association, 110(5), 464-472.
Teal, C. R., Shada, R. E., Gill, A. C., Thompson, B. M., Frugé, E., Villarreal, G. B., & Haidet, P. (2010). When best intentions aren't enough: Helping medical students develop strategies for managing bias about patients. Journal of general internal medicine, 25 Suppl 2(Suppl
Thomas, B., & Booth-McCoy, A. N. (2020). Blackface, implicit bias, and the informal curriculum: Shaping the healthcare workforce, and improving health. Journal of the National Medical Association, 112(5), 533-540.
Thomas, E. V. (2018). “Why even bother; they are not going to do it?” The structural roots of racism and discrimination in lactation care. Qualitative Health Research, 28(7), 1050-
Thomas, M. D., Michaels, E. K., Darling-Hammond, S., Nguyen, T. T., Glymour, M. M., & Vittinghoff, E. (2020). Whites’ county-level racial bias, COVID-19 rates, and racial inequities in the United States. International Journal of Environmental Research and Public Health, 17(22), Article 8695. https://doi.org/10.3390/ijerph17228695
Tsai, J. W., & Michelson, C. D. (2020). Attitudes toward implicit bias and implicit bias training among pediatric residency program directors: A national survey. The Journal of
Pediatrics, 221, 4-6. https://doi.org/10.1016/j.jpeds.2020.01.002
van Ryn, M., Hardeman, R., Phelan, S. M., PhD, D. J. B., Dovidio, J. F., Herrin, J., Burke, S. E., Nelson, D. B., Perry, S., Yeazel, M., & Przedworski, J. M. (2015). Medical school experiences associated with change in implicit racial bias among 3547 students: A medical student CHANGES study report. Journal of General Internal Medicine, 30(12), 1748–1756. https://doi.org/10.1007/s11606-015-3447-7
Wadhera, R. K., Wadhera, P., Gaba, P., Figueroa, J. F., Maddox, K. E. J., Yeh, R. W., & Shen, C. (2020). Variation in COVID-19 hospitalizations and deaths across New York City boroughs. JAMA, 323(21), 2192-2195. https://doi.org/10.1001/jama.2020.7197
Walkup, J. T., McAlpine, D. D., Olfson, M., Labay, L. E., Boyer, C., & Hansell, S. (2000).
Patients with schizophrenia at risk for excessive antipsychotic dosing. The Journal of
Clinical Psychiatry, 61(5), 344–348. https://doi.org/10.4088/jcp.v61n0504
White III, A. A., & Stubblefield-Tave, B. (2017). Some advice for physicians and other clinicians treating minorities, women, and other patients at risk of receiving health care disparities.
Journal of Racial and Ethnic Health Disparities, 4, 472-479.
White III, A. A., Logghe, H. J., Goodenough, D. A., Barnes, L. L., Hallward, A., Allen, I. M., ... & Llerena-Quinn, R. (2018). Self-awareness and cultural identity as an effort to reduce bias in medicine. Journal of Racial and Ethnic Health Disparities, 5, 34-49.
Zebib, L., Strong, B., Moore, G., Ruiz, G., Rattan, R., & Zakrison, T. L. (2019). Association of racial and socioeconomic diversity with implicit bias in acute care surgery. JAMA Surgery, 154(5), 459–461. https://doi.org/10.1001/jamasurg.2018.5855
Zestcott, C. A., Blair, I. V., & Stone, J. (2016). Examining the presence, consequences, and reduction of implicit bias in health care: A narrative review. Group Processes & Intergroup Relations, 19(4), 528-542. https://doi.org/10.1177/1368430216642029